- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
AI Capable of Detecting PAH Associated With Congenital Heart Disease
Congenital heart disease and pulmonary arterial hypertension (PAH) associated with congenital heart disease can be immediately detected using chest radiograph-based artificial intelligence (AI), a study found.
Artificial intelligence (AI) based on chest radiographs was able to detect congenital heart disease (CHD) and pulmonary arterial hypertension (PAH) associated with CHD (PAH-CHD) automatically. According to a study published in the European Journal of Radiology, this could help radiologists improve their diagnostic accuracy.
PAH is a frequent complication of CHD, which is the most common congenital defect with a high morbidity and mortality in children. Management of PAH and CHD is reliant on identifying them early, and chest radiography is a common measure to catch CHD. AI has been used for classifying and interpreting chest radiographs in the past with other cardiorespiratory issues, such as COVID-19. This study aimed to assess whether AI would be able to diagnose CHD and PAH based on a radiograph dataset.
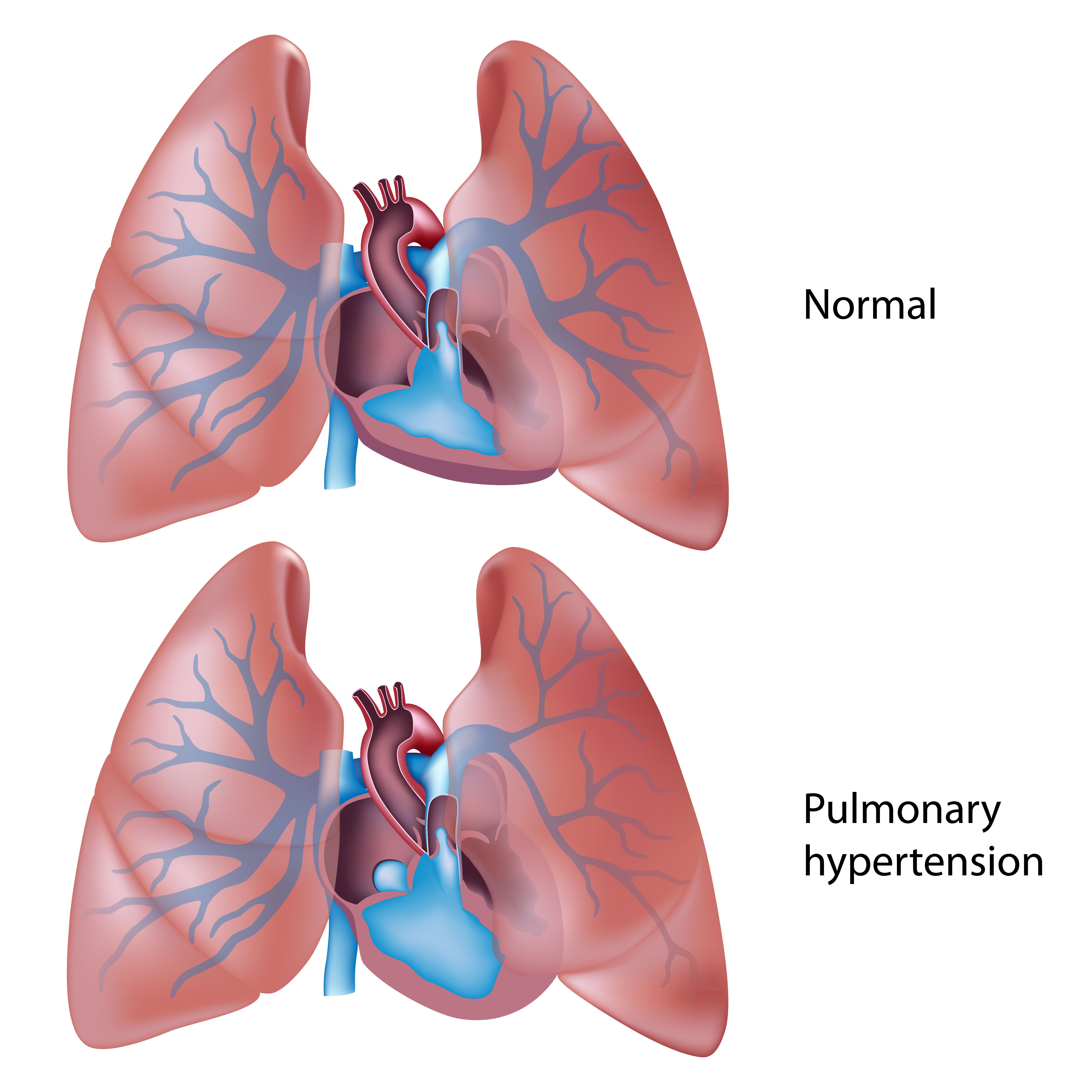
Pulmonary arterial hypertension | Image credit: Alila Medical Media - stock.adobe.com
This was a retrospective study including patients who had CHD from January 2018 to February 2022. All patients were included if they were aged younger than 18 years, had no previous cardiac surgery, had available information about the status of PAH related to CHD, and had available frontal chest radiographs. Controls were frontal chest radiographs in children who did not have CHD.
Several AI models were used to compare classification performance, with 330 images used to conduct a reader study. All radiologists read the images twice, and the 5 radiologists performed the diagnosis. There were 3 junior radiologists with at least 3 years of experience and 2 senior radiologists with at least 8 years of experience included in the reading study. Half of the images presented were also accompanied by the AI classification. After 1 month, the radiologists returned to take a look at the images again, but this time, the AI classification was provided for the other half of the images. The researchers of this study compared the performance of the radiologists with and without the AI assistance.
There were 3255 radiographs included in this study, of which 1174 were from children with CHD and 2081 were from those without CHD. There were 1032 non-PAH radiographs and 142 PAH radiographs of the 1174 radiographs that had CHD. There were 4 AI models used in the study. ResNet18 was used to identify CHD and PAH in this analysis as it had the highest sensitivity, specificity, and area under curve (AUC) for both.
Junior radiologists had AUCs of 0.670-0.809 and senior radiologists had AUCs of 0.803-0.858 when diagnosing CHD. Sensitivity ranged from 0.461 to 0.721 for junior radiologists and 0.903 to 0.927 for the senior radiologists, which was lower than the AI’s sensitivity of 0.970. Specificity was also higher in the AI model at 0.982 compared with a range of 0.703 to 0.879 in 4 of the radiologists; a junior radiologist had a comparable specificity of 0.988.
The AI model was found to have a significantly higher AUC of 0.778 compared with a junior radiologist (0.577) and was comparable to the other radiologists who had a range of 0.610 to 0.688 when diagnosing PAH. The AI model had higher sensitivity of 0.632 compared with a junior radiologist who had a sensitivity of 0.316 but was comparable to the other radiologists who had a sensitivity range of 0.526 to 0.632. The specificity was also significantly higher in the AI model at 0.925 compared with 2 junior and 1 senior radiologist who had a range of 0.534 to 0.904 and slightly higher for the remaining radiologists who had a specificity of 0.706 to 0.712.
For both CHD and PAH diagnosis, all radiologists had an increase in sensitivity, specificity, and AUC when using AI assistance.
There were some limitations to this study. This study took place in a single center, which could limit generalizability. Echocardiography was used to diagnose PAH but cardiac catheterization was not used. There was a serious imbalance between positive and negative samples of PAH, which could have affected how well the AI model did in identification. There was a small number of some specific CHD patients.
The researchers concluded that AI models based on chest radiographs had good performance when diagnosing CHD and PAH. AI models had better sensitivity, specificity, and AUC compared with radiologists and radiologists also benefitted when using AI recommendations.
“Such a chest radiograph-based AI model could assist in the automatic diagnosis of CHD and PAH-CHD, thereby contributing to early treatment and improving patient outcomes,” the authors wrote.
Reference
Han PL, Jian L, Cheng JL, et al. Artificial intelligence-assisted diagnosis of congenital heart disease and associated pulmonary arterial hypertension from chest radiographs: a multi-reader multi-case study. Euro J Radiolog. Published online December 26, 2023. doi:10.1016/j.ejrad.2023.111277
Echocardiographic Assessment Shows Promise as Risk Predictor in PAH
August 29th 2025Close to 40% of patients with right heart failure and pulmonary arterial hypertension (PAH) who remain critically ill and require admittance to the intensive care unit die within 1 year of that hospitalization.
Read More
Tricuspid Regurgitation Reliable Prognostic Indicator of PAH Severity
August 13th 2025Despite knowledge of the benefits of right heart hemodynamic measures for evaluating patient prognosis in the setting of pulmonary arterial hypertension (PAH), gaps remain in a defined role for tricuspid regurgitation as it relates to echocardiographic phenotype.
Read More
Lung Transplant Referrals Lag for High-Risk Patients With PAH
July 18th 2025Despite recommendations on early referral for lung transplantation in cases of pulmonary arterial hypertension (PAH), there is a lack of in-depth understanding of this current landscape; in this analysis, clinical parameter data were used to compare outcomes between patients who were and were not referred for lung transplantation.
Read More
