- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Adjuvant Chemotherapy Associated With Increased Survival Rate in Rectal Cancer
Patients who used adjuvant chemotherapy were found to have a higher survival rate after achieving complete pathological response.
Patients with rectal cancer who achieved complete pathological response (pCR) were found to have a higher survival rate when using adjuvant chemotherapy (ACT) thereafter, according to a review published in the International Journal of Colorectal Disease.1 This could indicate that ACT is beneficial for all patients with rectal cancer.
Colorectal cancer, when diagnosed in younger patients, is often aggressive and is the number 1 cause of cancer death in patients aged 20 to 49 years.2 Locally advanced rectal cancer (LARC) presenting a significant challenge in this population. Neoadjuvant chemoradiotherapy is often the method of treatment for the cancer but only a minority of patients achieve pCR using this therapy and tumor recurrence remains high. pCR is defined as an absence of any tumor cells after neoadjuvant chemoradiotherapy and is associated with a lower rate of tumor recurrence and risk of death. However, it is unknown how ACT can help patients with pCR, even as the National Comprehensive Cancer Network recommends ACT for all patients. This review aimed to assess the effect of ACT on patients who had LARC and achieved pCR.
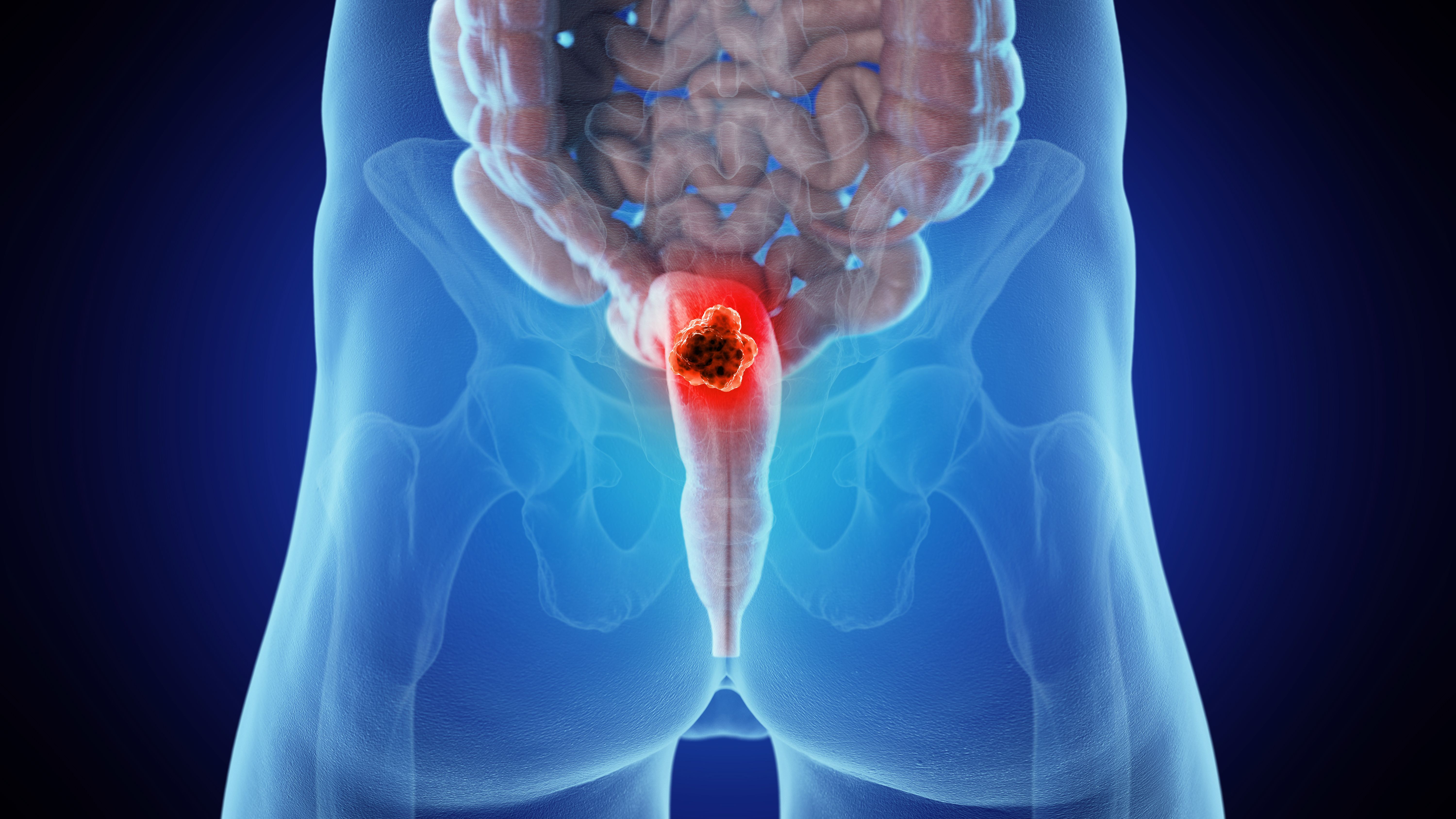
Rectal cancer can be aggressive in younger patients | Image credit: Sebastian Kaulitzki - stock.adobe.com
The researchers used PubMed, Embase, and Web of Science to search for studies that included patients diagnosed with rectal cancer who received neoadjuvant chemoradiotherapy; reported on overall survival (OS), disease-free survival (DFS), and relapse-free survival (RFS); and studies that compared ACT with no ACT. Studies were excluded if they were studies without results of interest, were single-arm clinical trials, or had overlapping populations.
Information including study design, gender, ACT, age, and country of study were extracted from the articles. A quality assessment was also undertaken to confirm the validity of the included studies.
There were 34 studies including 31,558 patients that were included in this review, of which 11,804 used ACT and 19,754 did not. The median age ranged from 52.9 to 65.7 years and most of the patients were at clinical stage II. Follow-up ranged from 35 to 120 months.
Patients using ACT had a prolonged OS compared with those who didn’t use ACT (HR, 0.75; 95% CI, 0.60-0.94). The OS was statistically improved in the ACT group in the 5-year analysis as well (OR, 1.65; 95% CI, 1.21-2.24). DFS was analyzed in 13 of the studies with 1809 patients included in the intervention group and 1927 in the control group. There was no significant affect on DFS in the 5-year analysis (OR, 1.19; 95% CI, 0.82-1.74).
There were 11 studies that included RFS with 1703 in the ACT group and 1348 in the control group. The HR was found to be 1.10 (95% CI, 0.87-1.40) and the 5-year analysis found no statistical significance (OR, 1.08; 95% CI, 0.78-1.51). Overall, 13 of the studies were considered good quality.
There were some limitations to this study. There were a lack of prospective randomized controlled trials that included the necessity of ACT for patients with rectal cancer who had achieved pCR, as all studies included were retrospective cohort studies. A multivariate analysis could not be conducted and could limit generalizability. Differences in DFS and RFS may not have been detected due to differences in follow-up times.
ACT was found to significantly improve OS in rectal cancer in patients who had pCR even though there was no significant improvement in either DFS or RFS. However, the improvement to OS makes ACT worthy of consideration for patients.
References
- De Moraes FCA, Kelly FA, Souza MEC, Burbano RMR. Impact of adjuvant chemotherapy on survival after pathological complete response in rectal cancer: a meta‑analysis of 31,558 patients. Int J Colorectal Dis. 2024;39:96. doi:10.1007/s00384-024-04668-x
- Rosenberg A. What’s behind rising colorectal cancer rates in young adults? City of Hope. March 11, 2024. Accessed June 25, 2024. https://www.cityofhope.org/whats-behind-rising-colorectal-cancer-rates-in-young-adults
