
- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Addressing Primary and Secondary Prevention of Osteoporosis-Related Fractures
Andrea J. Singer, MD, FACP, CCD
Departments of Obstetrics and Gynecology and Medicine, MedStar Georgetown University Hospital and Georgetown University Medical Center, Washington, DC, USA
David J. Harrison, PhD
Global Health Economics, Amgen Inc., Thousand Oaks, CA, USA
Burden of disease: Initial and secondary fractures
Osteoporosis is a bone disease that develops when bone mineral density (BMD) and bone mass decrease, which can lead to decreased bone strength.1 Clinical features of postmenopausal osteoporosis include low BMD and deterioration of bone structure, which cause bone fragility and increased fracture risk.2 Because osteoporosis is an asymptomatic disease, patients often are undiagnosed until they experience a fracture, which may lead to hospitalization.3,4 In fact, between 2000 and 2011, there were 4.9 million hospitalizations for osteoporosis-related fractures in women ages 55 and older at a cost of $5.1 billion per year.5 As a result, screening, diagnosis, and treatment for osteoporosis are crucial.
Osteoporosis is a disease that affects both men and women.1 One in two women and up to one in four men over the age of 50 will have a fracture related to osteoporosis in their remaining lifetime.2,6 However, the risk of fractures can be reduced.5,7 Bone loss occurs silently and progressively, often making a first fragility fracture the first sign of osteoporosis.4,8 With primary prevention, the risk of initial fracture in people with osteoporosis who are at a high risk for osteoporosis-related fracture can be reduced. High-risk patients can be identified through risk factors, BMD testing, and fracture risk assessment tools.5 The most common BMD test is a dual-energy X-ray absorptiometry (DXA), which is generally used for screening and diagnosis of osteoporosis.1 The Fracture Risk Assessment Tool (FRAX™*), which combines BMD and other clinical risk factors to calculate an individual’s probability of fracture over 10 years, can also be used to predict fracture risk and indicate need for pharmacologic therapy for osteoporosis.7
An initial fracture is associated with an 86% increased risk of a subsequent fracture.9,10 Therefore, secondary prevention of further osteoporosis-related fractures through diagnosis and treatment among postmenopausal women is important.11 In addition to proper nutrition, lifestyle changes, exercise, and fall prevention, there are medications to treat osteoporosis.1
However, despite a range of treatment options and guidelines, rates of osteoporosis testing, diagnosis, and treatment among postmenopausal women are low.12-15 For example, less than half of female patients between the ages of 67 and 85 received a BMD test or drug prescription to treat osteoporosis within 6 months of fractures, as reported per Medicare Quality Measures.16,† Clearly, there are gaps in care in patients with osteoporosis at a high risk for fracture in both primary and secondary prevention of osteoporotic fractures, which may be increasing plans’ exposure to the high cost of fractures.12-17
In patients with osteoporosis at a high risk of fracture: Primary and secondary prevention of osteoporosis-related fractures
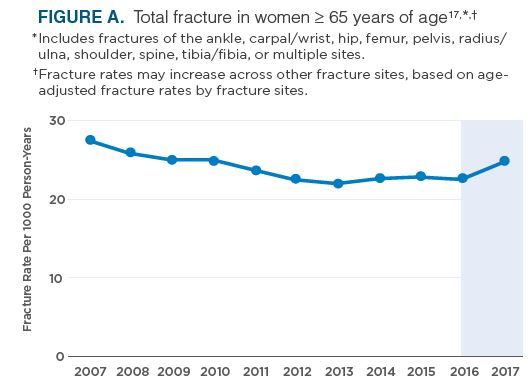
Osteoporosis-related fracture rates are on the rise.17 A retrospective analysis of the Optum Research Database from January 1, 2017 to May 31, 2017 in US commercial and Medicare plan members found that fracture rates among women ≥ 65 years of age declined from 2007 to 2013 and then plateaued until 2016.17 However, beginning in 2016, fracture rates increased across various fracture sites, including spine and multiple-site fractures (Figure A).17
Increased age- and sex-adjusted US fracture rates support the global call to action to increase screening and treatment of osteoporosis in older adults.17
*FRAX is a trademark owned by the International Osteoporosis Foundation.
†Based on data from 1/1/2018-12/31/2018.16
In patients with osteoporosis at a high risk for fracture, both new and subsequent fractures are costly over time14,15
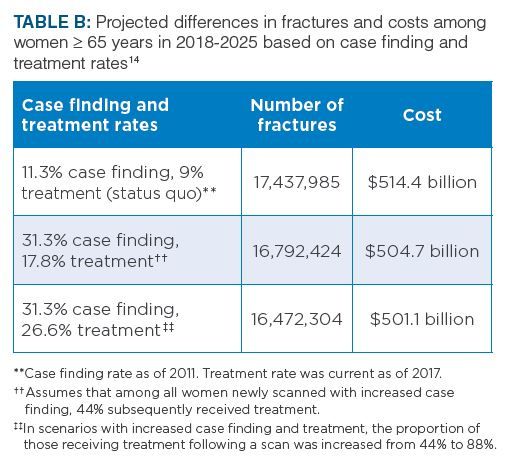
As the U.S. population continues to age and grow, the annual number of fractures among women ≥ 65 years of age is expected to increase. A microsimulation forecasting model projected that the incidence of osteoporosis-related fractures among US women ≥ 65 years of age would increase 68% from 2018 to 2040 (Table A).14 However, if case finding and treatment rates increase, the projected number of fractures and costs would decrease (Table B).14
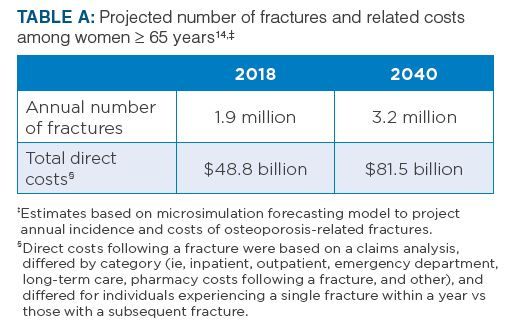
These projections assume that patients would be treated with available branded or generic products.14 Treatment effectiveness of included drugs was based on a meta-analysis of clinical trials and adjusted for adherence during each 1-year period.14
Osteoporosis-related fractures require considerable healthcare resource utilization.15 An analysis of administrative medical claims data from a Medicare Limited Data Set for a Medicare Fee-for-Service (FFS) population in 2015 found that the incremental annual direct medical cost in the 12-month period beginning with the new osteoporosis-related fracture (defined as those fractures that were newly diagnosed and not associated with a high-trauma event) was more than $21,800 than the costs incurred in the 12-month period prior to the fracture for the same beneficiaries.15 This figure includes amounts paid by Medicare and beneficiary cost sharing.15 Similarly, the estimated risk-adjusted incremental medical cost to Medicare of a subsequent fracture over the 180-day period following a new osteoporosis-related fracture was more than $20,700 (95% confidence interval: $19,900 to $21,800).15,§§
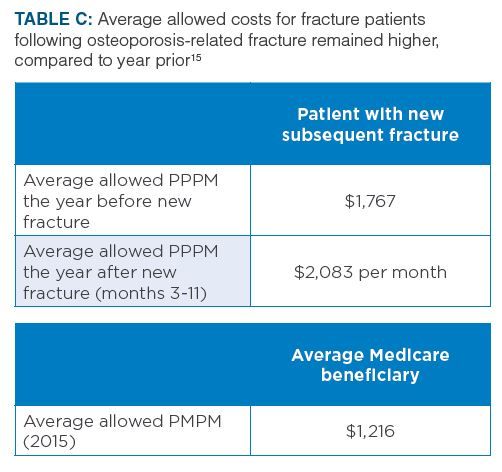
In the same analysis, patients with new fractures had higher average allowed per patient per month (PPPM) medical costs in the year before the new osteoporosis-related event compared with the 2015 average allowed per member per month (PMPM) for Medicare FFS patients ($1,767 compared with $1,216, after adjusting for differences in sex and age and trending to 2015 using Medicare cost trends).15
§§ Regression models were used to quantify the incremental cost of subsequent fractures by comparing costs in the 180-day period following a subsequent fracture for beneficiaries who have subsequent fracture to a similar 180-day period for beneficiaries without a subsequent fracture. The model analysis was based on historical practice patterns and treatments that may change over time, and experience may vary from the estimates in these results for many reasons.15
Costs for fracture patients continued to remain increased.15 Average allowed costs for fracture patients after the osteoporosis-related fracture remained higher compared to the year prior to the fracture: $2,083 per month in months 3 through 11 compared with $1,767 per month, after the year-by-year adjustment in cost data (Table C).15
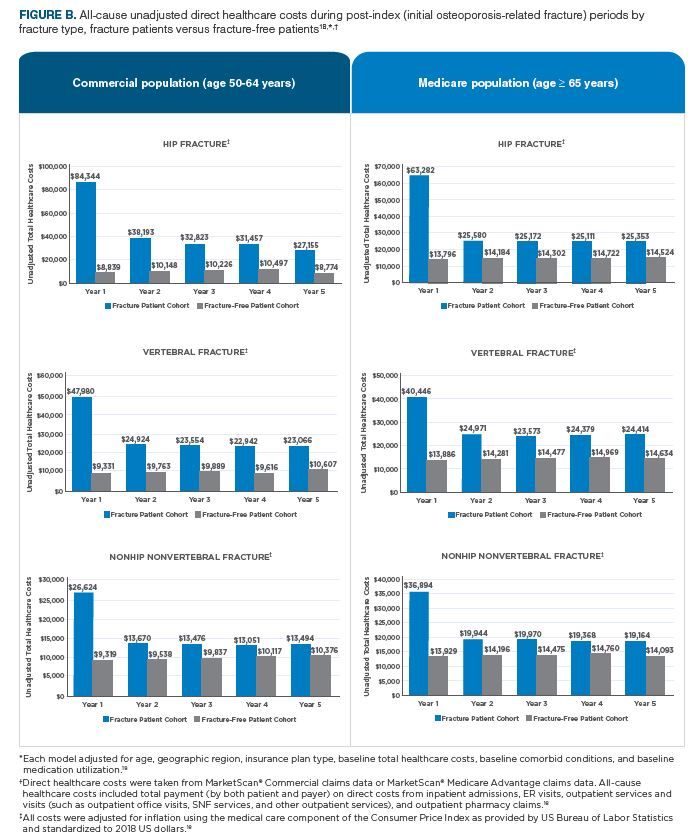
Even five years after a fracture, patients still have higher healthcare costs compared with patients without fractures.18 A separate analysis of claims data from the MarketScan® Commercial and Medicare databases that included women ≥ 50 years of age with incident osteoporosis-related fracture from 2008 to 2016 found that hip, vertebral, and nonhip nonvertebral (NHNV) fracture (excluding fractures of the skull, toes, and fingers) patients had higher mean total all-cause healthcare costs* across all 5 years after fracture in both commercial and Medicare populations (Figure B) when compared with demographically matched fracture-free patients.18
Costs for hip and vertebral fractures were each greater than costs for NHNV fractures.18 While the mix of fracture patients was evenly distributed across the Medicare population (hip: N=44,008; vertebral: N=43,175; NHNV: N=47,082), NHNV fractures were more common than hip and vertebral fractures among the commercial population (hip: N=5,329; vertebral: N=16,550; NHNV: N=70,046).18
In years 2 through 5 post osteoporosis-related fracture, vertebral fracture direct costs among patients ≥ 50 years of age were comprised of inpatient, outpatient, pharmacy, and ER-related costs.18
Gaps in testing, screening, and treatment
Once a patient is diagnosed with osteoporosis, their risk of fracture can be reduced with lifestyle modification and FDA-approved osteoporosis treatments.1,7,13
Additionally, DXA testing and diagnosis of osteoporosis declined between 2009 and 2014 among women who were Medicare FFS beneficiaries aged 65 and older.19 In 2014, the rate of DXA testing in this population was 11.3%, which may be in part due to a declining reimbursement rate.19 Between 2006 and 2015, Medicare reimbursement for office-based scans dropped 70%, from $139 in 2006 to $42 in 2015.19 As a possible result, some DXA facilities closed, which may have potentially led to decreased patient access to diagnostic services.19,20
While important in primary prevention of osteoporosis-related fractures in patients with osteoporosis at a high risk for fracture, screening, diagnosis, and osteoporosis treatment are crucial for secondary prevention of osteoporosis-related fractures.1,5,11 Following initial fracture, postmenopausal women are 5 times more likely to suffer another fracture within the first year, which is a risk that remains elevated over time.21,†
*All-cause healthcare costs included total payment (by both patient and payer) on direct costs from inpatient admissions, ER visits, outpatient services and visits (such as outpatient office visits, SNF services, and other outpatient services), and outpatient pharmacy claims.18
†Data represent a population-based study of 4,140 postmenopausal women aged 50-80 years.21
An initial osteoporosis-related fracture is associated with an 86% increased risk of a subsequent fracture.9,10
Various organizations have recognized the importance of osteoporosis testing and treatment.16,22 Both HEDIS and Medicare Part C STAR Ratings include a measure to rate quality of osteoporosis care: “Osteoporosis Management in Women Who Had a Fracture.”16,22 2020 STAR Rating reflects low testing and treatment rates, as only 48% of patients received testing or treatment within 6 months of fracture.16,22
The average 2020 Medicare STAR rating for the “Osteoporosis Management in Women Who Had a Fracture” Part C measure was 3.1/5 stars, which indicates that 52% of female patients ages 67 to 85 did not receive a BMD test or prescription for a drug to treat osteoporosis within 6 months of a fracture.16 Plans included in the Part C ratings include 1876 Cost Employer/Union Only Direct Contract Local Coordinated Care Plans, Employer/Union Only Direct Contract Private Fee-for-Service, Local Coordinated Care Plan, Medical Savings Account, Private Fee-for-Service, Regional Coordinated Care Plan, Religious Fraternal Benefit Private Fee-for-Service, and Religious Fraternal Benefit Local Coordinated Care Plan.16 This measure has been one of the lowest ranking Medicare Part C quality measures at health plans over the last 4 years (2017-2020).23
A call for diagnosis of osteoporosis
The low rates of osteoporosis diagnosis and treatment, particularly following a fracture, highlight the need for improved care coordination as patients transition from inpatient to ambulatory care.11 Leading organizations call for screening, diagnosis, and treatment of patients with osteoporosis at a high risk for fracture.11
The American Society for Bone and Mineral Research has called for improved care coordination for people ≥ 65 years with a hip or vertebral fracture and for insurers to cover the most effective services for improving the diagnosis and treatment of those at the highest risk for osteoporosis and fractures.11,24 The American Association of Clinical Endocrinologists (AACE)/American College of Endocrinology (ACE) and the National Osteoporosis Foundation (NOF) call for osteoporosis and fracture prevention.7,25
The 2020 AACE/ACE Clinical Practice Guidelines for the Diagnosis and Treatment of Postmenopausal Osteoporosis recommend that all postmenopausal women aged ≥ 50 years undergo clinical assessment for osteoporosis and fracture risk, including a detailed history, physical examination, and clinical fracture risk assessment with FRAX™ or other fracture risk assessment tool.7
BMD testing is a key element in diagnosing osteoporosis and monitoring therapy in people with osteoporosis at a high risk for fracture.7 The gold standard for measuring BMD is dual-energy X-ray absorptiometry (DXA).7 The AACE/ACE 2020 Guidelines recommend BMD testing for the following women7:
- Women ≥ 65 years
- Younger postmenopausal women at increased risk for bone loss and fracture, based on analysis of fracture risk
For patients on treatment or with a baseline evaluation near a fracture intervention threshold, BMD testing every 1 to 2 years is often appropriate.7
BMD results should be combined with other clinical risk factors for fractures for accurate assessment of fracture risk and to guide treatment decisions.7,26 This can be accomplished using FRAX™, as it combines BMD and other clinical risk factors, enabling it to predict fracture risk better than clinical risk factors or BMD alone.7,26 Other risk assessment tools beside DXA should be available to providers as well.7,26
The Best Practice Framework from the Capture the Fracture campaign addresses secondary fracture prevention and benchmarks fracture liaison services based on various measures including patient evaluation, post-fracture assessment timing, and identification and secondary fracture prevention for previously unrecognized vertebral fractures.27 Electronic health record databases can be used to identify patients following an osteoporosis-related fracture.28,29
Treatment is supported by guideline recommendations
In order to treat osteoporosis and reduce the risk of future fractures, guidelines recommend pharmacological treatment in several patient types.7
The AACE/ACE 2020 Guidelines strongly recommend pharmacologic therapy for patients with7:
- Osteopenia or low bone mass and a history of fragility fracture of the hip or spine
- A T-score, which describes bone mineral density, of -2.5 or lower in the spine,
femoral neck, total hip, or 1/3 radius - A T-score between -1.0 and -2.5 if the FRAX™ 10-year probability for major osteoporosis-related fracture is ≥ 20% or the 10-year probability of hip fracture is ≥ 3% in the U.S. or above the country-specific threshold in other countries or regions
The NOF recommends initiation of pharmacologic treatment in25:
- Those with hip or vertebral (clinical or asymptomatic) fractures
- Those with T-scores ≤ −2.5 at the femoral neck, total hip, or lumbar spine by DXA
- Postmenopausal women and men age 50 and older with low bone mass (T-score between −1.0 and −2.5, osteopenia) at the femoral neck, total hip, or lumbar spine by DXA and a 10-yearhip fracture probability ≥ 3% or a 10-year major osteoporosis-related fracture probability ≥ 20% based on the USA-adapted WHO absolute fracture risk model (FRAX™)
Help protect members with osteoporosis at a high risk for fracture
Providers need to be fully empowered to identify patients with osteoporosis. First, access and reimbursement for DXA should be increased to help prevent fractures. If DXA were reimbursed at the rate it is in the hospital setting, DXA utilization was estimated to be increased to 31.3% of patients, which would double treatment to 26.6% of women ages 65 years and older.14 Even with spending on DXA testing, cumulative projected savings to Medicare from 2018 to 2040 could lead to a cost savings of $41.9 billion.14
Second, access to treatment is needed, and access should not be uniform across all patients.
The AACE/ACE 2020 Guidelines state that physicians should individualize treatment decisions based on patient preferences and circumstances and level of fracture risk.7,11 Some patients who are at very high fracture risk may require more aggressive treatment to achieve an acceptable level of fracture risk.7,11
Therefore, utilization management should allow for guideline-recommended therapy and risk stratification.
In order to reduce fracture risk and lower total healthcare costs, it is important to ensure persistent use of osteoporosis medication.30,*
There are several potential implications of restricting access for patients within the FDA-approved indication. Clinically appropriate patients may be denied or delayed access despite low treatment and diagnosis rates in postmenopausal osteoporosis, which may lead to increased fracture rates.16,22 Lower quality ratings are associated with lower treatment rates.16,22
*Data based on female Medicare beneficiaries diagnosed with osteoporosis and initiated on osteoporosis medication January 1, 2009, through June 30, 2011.30
Summary
Osteoporosis is an asymptomatic disease that can remain undiagnosed until patient fracture occurs, which may lead to hospitalization.3,4 Despite a range of treatment options and guideline recommendations, rates of testing, diagnosis and treatment among postmenopausal women are low.12-15 There is a clear burden of osteoporosis on payers with the number of osteoporosis-related fractures increasing in the U.S., increasing costs and health resource utilization.14,15
For patients with osteoporosis at a high risk for fracture, screening, DXA testing, diagnosis, and osteoporosis treatment are essential for both primary and secondary prevention of osteoporosis-related fracture.5,11 Various organizations recognize the importance of osteoporosis testing and treatment, and clinical guidelines call for specific measures to be taken with patients with osteoporosis at a high risk for fracture.7,11 Access and reimbursement for DXA testing should be increased to help prevent fractures.7,14 Appropriate treatments should be made available to eligible members, allowing physicians to take individual patient needs into account, including the degree of fracture and fracture risk.7,14 Payer evaluation of their utilization management criteria for postmenopausal osteoporosis medications will aid in the management of member populations with osteoporosis and their associated costs.
Disclosures
Dr. Singer does paid consulting in research and quality improvement through Radius Health, Inc, and UCB. She also works in a paid consulting and medical advisory capacity with AgNovos Health Care, Amgen Inc., Radius Health, Inc., and UCB. She has had speaking engagements through Amgen Inc., and Radius Health, Inc. Dr. Singer is also on the Board of Trustees for the National Osteoporosis Foundation in a non-remunerative role.
References:
1. National Institute of Arthritis and Musculoskeletal and Skin Diseases. Overview of Osteoporosis.
https://www.bones.nih.gov/health-info/bone/osteoporosis/overview. Accessed March 23, 2021.
2. U.S. Department of Health and Human Services. Bone Health and Osteoporosis: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Office of the Surgeon General, 2004.
3. Tu KN, Lie JD, Wan CKV, et al. Osteoporosis: a review of treatment options. P T. 2018;43:92-104.
4. National Osteoporosis Foundation. What Is Osteoporosis and What Causes It? https://www.nof.org/patients/what-is-osteoporosis/. Accessed March 23, 2021.
5. Singer A, Exuzides A, Spangler L, et al. Burden of illness for osteoporotic fractures compared with other serious diseases among postmenopausal women in the United States. Mayo Clin Proc. 2015;90:53-62. doi: 10.1016/j.mayocp.2014.09.011.
6. National Osteoporosis Foundation. Just for Men. https://www.nof.org/preventing-fractures/general-facts/just-for-men/. Accessed March 23, 2021.
7. Camacho PM, Petak SM, Binkley N, et al. American Association of Clinical Endocrinologists/American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis—2020 update. Endocr Pract. 2020;26(suppl. 1):1-46.
8. van Oostwaard M. Osteoporosis and the Nature of Fragility Fracture: An Overview. In: Hertz K, Santy-Tomlinson J, eds. Fragility Fracture Nursing: Holistic Care and Management of the Orthogeriatric Patient. Cham, Switzerland; Springer; June 16, 2018. 1-13.
9. Kanis JA, Johnell O, De Laet C, et al. A meta-analysis of previous fracture and subsequent fracture risk. Bone. 2004;35:375-382.
10. Weaver J, Sajjan S, Lewiecki EM, Harris ST, Marvos P. Prevalence and cost of subsequent fractures among U.S. patients with an incident fracture. J Manag Care Spec Pharm. 2017;23:461-471.
11. American Society for Bone and Mineral Research. Call to action to address the crisis in the treatment of osteoporosis.
https://www.asbmr.org/Assets/d5139738-e1b3-4645-859a-96affc059ae3/636098972158530000/call-to-action-to-address-the-crisis-in-the-treatment-of-osteoporosis-final-003-pdf. Accessed March 23, 2021.
12. Boystov NN, Crawford AG, Hazel-Fernandez LA, et al. Patient and provider characteristics associated with optimal post-fracture osteoporosis management. Am J Med Qual. 2017;32:644-654.
13. Gillespie CW, Morin PE. Trends and disparities in osteoporosis screening among women in the United States, 2008-2014.
Am J Med. 2017;130:306-316.
14. Lewiecki EM, Ortendahl JD, Vanderpuye-Orgle J, et al. Healthcare policy changes in osteoporosis can improve outcomes and reduce costs in the United States. JBMR Plus. 2019;3:e10192.
15. Hansen D, Bazell C, Pelizzari P, Pyenson, B. Medicare cost of osteoporotic fractures: The clinical and cost burden of an important consequence of osteoporosis. Milliman Research Report. 2019;1-48.
16. Centers for Medicare & Medicaid Services. Medicare 2020 Part C & D Star Ratings Technical Notes. https://www.hhs.gov/guidance/sites/default/files/hhs-guidance-documents/Star%20Ratings%20Technical%20Notes%20%28Oct%2010%202019%29.pdf. Updated October 1, 2019. Accessed February 2, 2021.
17. Lewiecki EM, Chastek B, Sundquist K, et al. Osteoporotic fracture trends in a population of US managed care enrollees from 2007 to 2017. Osteoporos Int. 2020;31:1299-1304.
18. Data on file, Amgen; 2020.
19. Lewiecki EM, Adler R, Curtis J, et al. Hip Fractures and Declining DXA Testing: At a Breaking Point? Presented at American Society for Bone and Mineral Research Annual Meeting: September 16-19, 2016; Atlanta, Georgia, USA.
20. King AB, Fiorentino DM. Medicare payment cuts for osteoporosis testing reduced use despite tests' benefit in reducing fractures. Health Aff (Millwood). 2011;30:2362-2370.
21. van Geel TACM, van Helden S, Geusens PP, Winkens B, Dinant G-J. Clinical subsequent fractures cluster in time after first fractures. Ann Rheum Dis. 2009;68:99-102.
22. National Committee for Quality Assurance. Osteoporosis Testing and Management in Older Women (OTO, OMW).
https://www.ncqa.org/hedis/measures/osteoporosis-testing-and-management-in-older-women/. Accessed March 23, 2021.
23. Centers for Medicare and Medicaid Services. Fact Sheet - 2020 Part C and D Star Ratings. https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovGenIn/Downloads/2020-Star-Ratings-Fact-Sheet-.pdf. Accessed February 2, 2021.
24. Conley RB, Adib G, Adler RA, et al. Secondary fracture prevention: consensus clinical recommendations from a multistakeholder coalition. J Bone Miner Res. 2020;35:36-52.
25. Cosman F, de Beur SJ, LeBoff MS, et al. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25:2359-2381.
26. The International Society for Clinical Densitometry. 2010 Official Positions on FRAX®. https://iscd.app.box.com/s/4k35szskkiorkl5wm3ic2webouoc5rw2. 2010. Accessed March 23, 2021.
27. Akesson K, Marsh D, Mitchell PJ, et al. Capture the Fracture: a best practice framework and global campaign to break the fragility cycle. Osteoporos Int. 2013;24:2135-2152.
28. Miller AN, Lake AF, Emory CL. Establishing a fracture liaison service: an orthopaedic approach. J Bone Joint Surg Am. 2015;97:675-681.
29. Chow S. Health information technology is transforming osteoporosis care management. CareManagement. 2017;23:12-14.
30. Liu J, Guo H, Rai P, Pinto L, Barron R. Medication persistence and risk of fracture among female Medicare beneficiaries diagnosed with osteoporosis. Osteoporos Int.. 2018;29:2409–2417.
© 2021 Amgen Inc. All rights reserved. USA-785-81555
2 Commerce Drive
Cranbury, NJ 08512
AJMC®
All rights reserved.
