- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
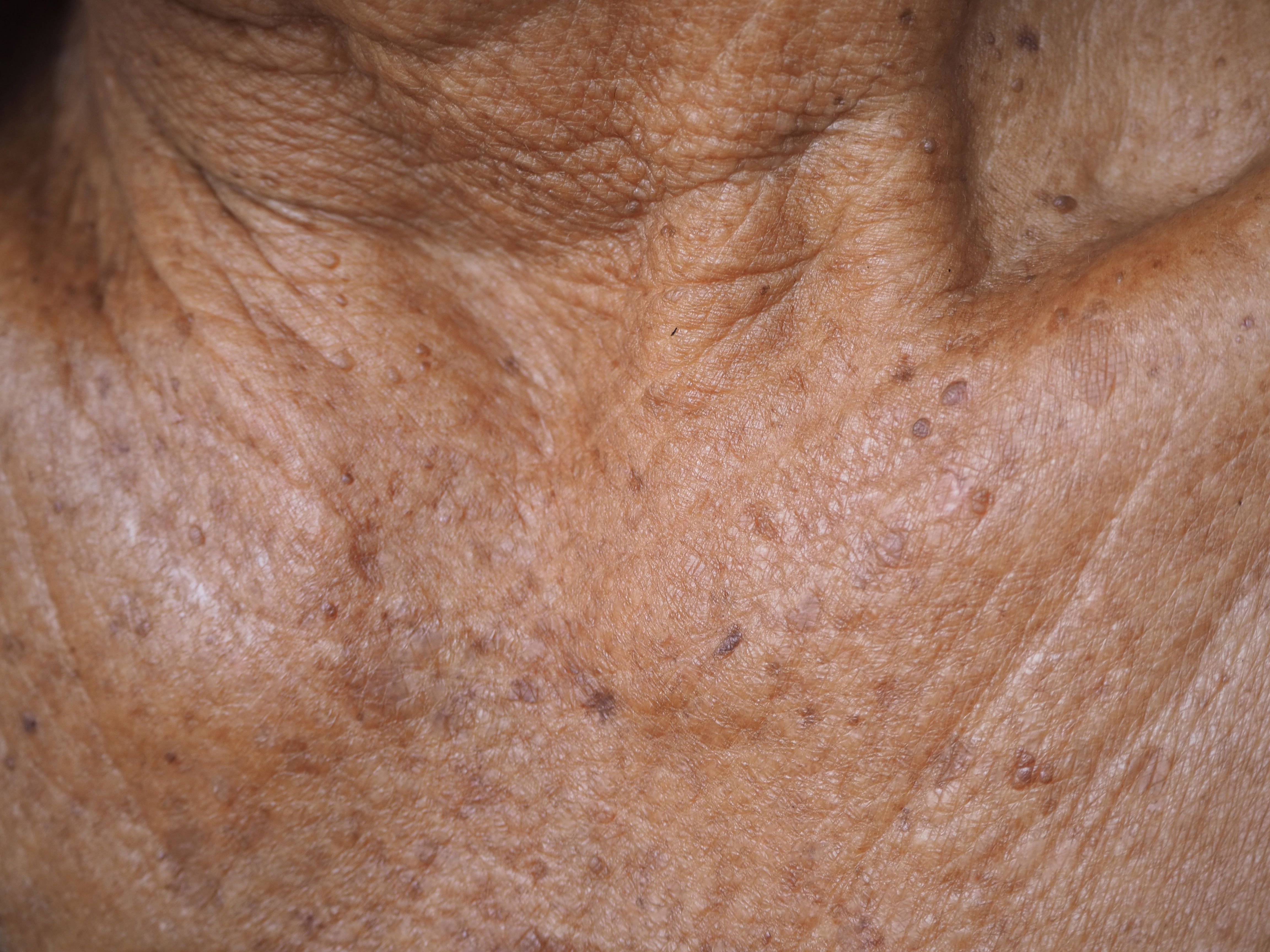
Actinic Keratoses Put Patients at Increased Skin Cancer Risk
This retrospective cohort study demonstrates the heightened risks individuals with actinic keratoses have for developing skin cancers.
A recent study published in JAMA Dermatology indicates that older patients with actinic keratoses (AKs) carry an increased risk melanoma, squamous cell carcinoma (SCC), and basal cell carcinoma (BCC). These results suggest the efficacy and value of using AKs as clinical markers for skin cancer at large.
Older individuals commonly develop premalignant skin lesions, known as AKs, because of significant UV exposure. Previous studies have demonstrated how patients with AKs may have heightened risks for developing certain skin cancers; however, despite these associations, no current guidelines encourage follow-up cancer monitoring for these patients. The authors of the present study mention how this lack could stem from insufficient data on this patient population that adequately tracks their clinical follow-up outcomes.
Actinic Keratosis Model | image credit: jaojormami - stock.adobe.com
To gain more knowledge in this area, the researchers retrospectively analyzed a random sample of Medicare beneficiaries aged 65 and older from 2009-2018. This group included 555,945 individuals who were treated for AKs and 481,024 with seborrheic keratoses (SKs) for comparison. None with a history of skin cancer were included. All eligible beneficiaries had at least 1 year between their entry into the data set and their first recorded AK or SK. Investigators assessed skin cancer risks for those with AKs, compared these risks with those with SKs, and evaluated patients’ first-recorded surgical treatment of skin cancer. Patients with AKs and SKs had average follow-ups of 5.6 and 4.5 years, respectively.
The analysis revealed that the absolute risk of any skin cancer developing after someone’s initial AK was 6.3% at 1 year (95% CI, 6.3%-6.4%), 18.4% at 3 years (95% CI, 18.3%-18.5%), and 28.5% at 5 years (95% CI, 28.4%-28.7%).
Compared with those with SKs, beneficiaries with AKs carried an overall increased risk of skin cancer (adjusted HR [aHR], 2.17; 95% CI, 2.15-2.19), which was observed in rates of melanoma (aHR, 1.67; 95% CI, 1.60-1.73), BCC (aHR, 1.85; 95% CI, 1.82-1.87), keratinocyte carcinoma (KC; aHR, 2.20; 95% CI, 2.18-2.22), and SCC (aHR, 2.63; 95% CI, 2.59-2.66).
The authors also conducted a dose-response analysis to compare outcomes in beneficiaries considered to have a higher burden of AKs with those considered to have lower AK burden. In total, 77,453 beneficiaries were characterized as having higher burden and 478,592 were characterized as having lower burden. Those with higher burden were noted to have a significantly higher risks of skin cancer (aHR, 1.74; 95% CI, 1.71-1.76), including melanoma (aHR, 1.48; 95% CI, 1.41-1.54) and KC (aHR, 1.63; 95% CI, 1.63-1.64), than those with lower burden.
There is still room to grow in this research. Among the limitations experienced in this study, the authors noted the generalizability of a cohort of individuals of 65 years and older. Although their results suggest the value of AKs as clinical biomarkers, and indicate the associations between AKs and vulnerability to skin cancers, future studies should consider younger populations for patients and clinicians to gain a more well-rounded understanding of the risks at play.
Reference
Mohr C, Li Y, Navsaria LJ. Skin cancers in Medicare beneficiaries with actinic keratoses. JAMA Dermatol. 2023;159(12):1368-1372. doi:10.1001/jamadermatol.2023.4266
