- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
Standards of Care Issues With Anticoagulation in Real-World Populations
Current guidelines recommend anticoagulants for reducing the risk of stroke in appropriate patients with nonvalvular atrial fibrillation (NVAF) and for the acute treatment of venous thromboembolism (VTE) and the prevention of recurrent VTE. Warfarin is the standard of care for both NVAF and VTE, yet International Normalized Ratio (INR) control remains suboptimal, even in the clinical trial setting. Maintaining INR within the recommended therapeutic range is associated with better outcomes in these distinct populations. In VTE, high rates of recurrence have been reported during the first few weeks of treatment, emphasizing the importance of surveillance during this time and of early optimization of anticoagulation therapy. The NVAF population tends to have more comorbidities and requires longer-term therapy. It is important to keep in mind that real-world patient populations are more complex than those in controlled studies. Patients with multiple comorbidities are particularly challenging, and physicians may focus on clinically urgent issues rather than anticoagulation optimization. Despite the many complexities associated with the use of warfarin, it remains a mainstay of anticoagulation therapy. Aligning financial incentives and improving care coordination are important factors in moving toward better outcomes for patients who need anticoagulation therapy. The increased focus on value-based care and evolving approaches to patient treatment could lead more physicians and payers to consider alternatives to warfarin, including the use of novel oral anticoagulants.
Am J Manag Care. 2014;20:S4-S9This article is the second in a 2-part series that summarizes the proceedings from a roundtable meeting conducted to discuss real-world considerations in nonvalvular atrial fibrillation and venous thromboembolism.
Warfarin is the oral anticoagulant with the highest level of evidence in long-term anticoagulation therapy, in both venous thromboembolism (VTE) and nonvalvular atrial fibrillation (NVAF).1,2 The standard of care in treating and reducing the risk of recurrent VTE may involve initial treatment with unfractionated heparin or low-molecular weight heparin (LMWH) and bridging to a vitamin K antagonist (VKA) such as warfarin.1 Compared with treatment of VTE, use of anticoagulants for reducing the risk of stroke in patients with NVAF tends to be longer-term, and patients are typically older and have more comorbidities. There are several inherent complexities with warfarin treatment, such as frequent international normalized ratio (INR) monitoring, dosing variability, numerous drug-drug interactions, and dietary restrictions.3 The introduction of novel oral anticoagulants (NOACs) has altered the treatment landscape, resulting in additional realworld considerations for practitioners and payers.
The content for this supplement is based on select study data as well as applicable discussion points that stemmed from the roundtable discussion entitled Research to Real-World Application: Considerations for Use of Health Economic and Outcomes Data in Anticoagulation. Faculty participants discussed research articles that provided information regarding the importance of INR control in VTE and NVAF populations and the difficulties in achieving a stable INR range. Data were presented that described factors associated with poor INR control and the relationship between INR control and outcomes. Also discussed were the complexities of warfarin therapy in clinical practice and how NOACs fit into anticoagulation therapy.
Anticoagulation Therapy and Reducing the Risk of Recurrent VTE
Current guidelines recommend anticoagulant therapy for appropriate patients with VTE events, depending on the location of the VTE event and patient risk factors, as determined by a physician.1 Previous studies have indicated that the incidence of recurrent VTE is highest during the first 1 to 3 weeks of treatment after the index event, suggesting that patients need to quickly receive and optimize anticoagulation therapy to minimize the risk of early recurrent VTE events.4-6
To formally examine the pattern of recurrent VTE risk, Limone and colleagues performed a meta-analysis of 15 randomized controlled trials (N = 27,237 in 31 treatment arms) of patients receiving at least 3 months of anticoagulation. The authors reported that in 68% of the 31 treatment arms, initial treatment of VTE consisted of unfractionated heparin or LMWH as a bridge to a VKA. Recurrent VTE rates were highest in the first week of treatment (0.29 events per person-year; 95% CI, 0.21- 0.37), and remained high over the next 3 weeks. After 5 weeks, risk decreased significantly (P <.007) and stabilized to 0.05 or fewer events per person-year (Figure 1).6 In a mixed linear model meta-regression on pooled data at 1 month, the recurrent VTE rate was 0.16 events per person-year lower among those who had a pulmonary embolism with or without deep vein thrombosis (DVT) than among the DVT-only population.6
The high recurrent VTE rates in the first 4 weeks emphasize the importance of surveillance during this time and of optimizing anticoagulation therapy as early as possible.6
Faculty participants expressed surprise at the high VTE recurrence rate, given that the patients were being treated with anticoagulation therapy. “It raises a lot of issues,” commented Edmund J. Pezalla, MD, MPH. The finding that the majority of VTE recurrences fall within the same critical period it takes INR to stabilize and patients to achieve therapeutic levels led some of the participant to note that the data support the use of medications in this population that do not require frequent monitoring of INR, such as NOACs. Jeffrey D. Dunn, PharmD, MBA, stated, “It just reinforces the use of the NOACs, quite frankly.” Several of the participants noted that it is now common in most markets for NOACs to be prescribed in secondary prevention of VTE.
Participants also noted that bridging requirements associated with warfarin in this population further complicate treatment and encourage the use of NOACs. “If we can use a NOAC, we avoid the bridging issue altogether,” noted Joseph E. Biskupiak, PhD, MBA. Geno J. Merli, MD, FACP, FHM, FSVM, explained that the bridging process is managed by his institution’s vascular program, which is responsible for scheduling appointments for INR monitoring to ensure that a patient has an INR between 2.0 and 3.0 for 2 consecutive days before the patient is handed off to his or her primary care physician. When considering tier placement for this category, pharmacy and therapeutics committees do consider the costs associated with bridging and rates of readmission, according to several of the participants.
The participants discussed the importance of having anticoagulation clinics for the prevention of readmissions. Without these clinics, transition of care becomes much more difficult, and patients are less compliant with their medications. Health systems include many different types of hospitals, however, and one approach to preventing readmissions may not work well with all hospitals. “Readmissions matter a lot. The biggest issue we have is, there are lots and lots of hospitals to work with, so one size does not fit all,” Dr Pezalla said. His system’s general approach is to train nurses and pharmacists working with patients on transitional care outside the hospital to reduce readmissions. Several of the participants commented that care at an anticoagulation clinic is generally not reimbursable. Hospital departments often fund their own clinics, assuming all the risk. In general, participants agreed that the lack of heterogeneity within systems affected their institutions’ ability to address readmissions of recurrent VTEs.
Anticoagulation Control and Outcomes in Atrial Fibrillation Patients
Sidebar
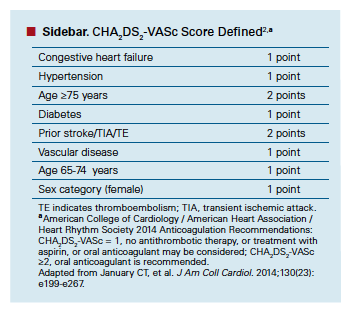
In NVAF, anticoagulant therapy is used for reducing the risk of stroke and systemic embolism and is longer term than in VTE. Also, the NVAF patient population tends to be older, has more comorbidities, and takes more medications for chronic conditions, introducing additional challenges to care. American College of Cardiology/American Heart Association/Heart Rhythm Society 2014 guidelines recommend use of an anticoagulant in patients with NVAF with a CHA2DS2-VASc score of 2 or more (see ),2 and in patients who have had a prior stroke or transient ischemic attack. Among those who use warfarin, maintaining INR within a therapeutic range (2.0-3.0) is critical to reducing the risk of stroke as well as bleeding. Guidelines recommend the use of NOACs as an alternative to warfarin.2
A meta-analysis by Wan et al conducted in 2008 highlighted the importance of INR management in AF patients receiving warfarin. Wan and colleagues collected data from 38 studies that included 27 retrospective studies, 5 prospective studies, and 15 randomized controlled trials (RCTs) of 33,976 patients with AF, and evaluated the relationship between INR control and the risk of major hemorrhage and thromboembolic events. The time in therapeutic range (TTR) ranged from 29% to 75%, and better INR control was observed in RCTs than in retrospective studies (64.9% vs 56.4%, respectively).7
In retrospective studies, which may better reflect realworld conditions, TTR was negatively correlated with major hemorrhage and thromboembolic events (r = —0.78; P = .006 and r = —0.88; P = .026, respectively). Linear regression of retrospective studies revealed that a 6.9% increase in TTR resulted in 1 less major hemorrhage event per 100 person-years, and an 11.9% increase in TTR reduced thromboembolic events by 1 event per 100 person-years. However, no linear relationships existed for RCTs. Based on the retrospective study results, Wan et al (2008) recommended a TTR goal of between 70% and 80% to optimize benefits and reduce harm for patients.7
Reacting to the data from Wan, faculty participants were not surprised with the observation that INR control was better in RCTs. They attributed this to the controlled conditions and close monitoring that patients experience in these clinical trials. Even in RCTs, however, INR control can be suboptimal, noted several of the participants. Participants also pointed out that some managed care systems are well coordinated and provide exceptional levels of INR control. “There are systems that probably do very well,” said Dr Biskupiak. “Their INR is actually better than we see in the studies.” Overall, the participants agreed that the real issue is finding a way for everyone to accomplish good INR control in their patients, rather than having disparities across systems. The participants also agreed that the negative correlation between TTR and risk of adverse events was logical and that they would be concerned if there were not such an association.
Patient Characteristics, Comorbidities, and INR Control
Patient populations in a real-world setting are often more complex than those included in controlled clinical studies, and this can affect the likelihood of achieving optimal INRs. In a longitudinal retrospective study, Nelson et al examined 23,425 NVAF patients who had received warfarin for at least 12 months. A multivariate analysis revealed that heart failure, diabetes, and previous stroke were associated with lower TTR (Figure 2).8 A second multivariate analysis demonstrated that a CHADS2 (Congestive heart failure, Hypertension, Age ≥75 years, Diabetes mellitus, prior Stroke, transient ischemic attack or thromboembolism [doubled]) score of 2 or higher was also associated with low TTR (adjusted odds ratio, 1.11; 95% CI, 1.04-1.18; P = .003). In general, the data showed that as CHADS2 score increased, TTR decreased. Because the patients in this study received specialized care at anticoagulation clinics, the authors suggested that anticoagulation control is likely more challenging in patients with comorbidities.8
Participants mentioned that when presented with a patient with multiple comorbidities, physicians evaluate the severity of each comorbidity and initially focus on the conditions that they deem to be more clinically urgent. Initiating anticoagulation therapy may not be a priority. Dr Merli stated, “We are talking about a risk of something versus you have this problem, and I am going to treat the problems first. And the risk? I am concerned about that, but first and foremost, I have to deal with the problems you have today.” One participant suggested that fear of comorbidities might lead providers to decide against prescribing an anticoagulant. Some panelists noted that physicians may target on the lower end of the INR range for complex patients to compensate for potential bleed risk.
The complexities with regard to managing patients with multiple comorbidities are closely tied to the concern of polypharmacy, according to the participants. Fadia T. Shaya, PhD, MPH, noted that it would be interesting to track more than just the diagnoses of the patient. Specifically, the medication history should be tracked to provide a more complete picture of the patient. Providing an example, Dennis B. Liotta, MD, MBA, added, “A diabetic patient is not a diabetic patient, right? If they are on 3 or 4 medications, that is a very different diabetic patient than one that is just on metformin.” Several participants pointed out the complexities of managing this patient population, and the challenges associated with compliance. Tomás Villanueva, DO, MBA, FACPE, SFHM, said, “If you are looking at a diabetic patient who has had a history of heart failure, there is a good chance that patient is taking 7 to 10 drugs.” Dr Pezalla commented that the physician’s fear is likely centered on the patient’s ability to self-manage. “Part of the problem is not that the physician cannot manage the 8 drugs the patient is on,” he said. “They are concerned about the patient managing the 8 drugs.” Some participants noted that NOACs may have an advantage in these complex patients because NOACs do not require frequent monitoring and have fewer drug-drug interactions. However, the fact that warfarin requires frequent monitoring is viewed as a positive attribute by some providers, according to Dr Liotta. “Anecdotally, you hear that some physicians like the fact that patients are coming in and you know where they are and where their INRs are so you know if they are being compliant, and there are more touch points,” he said. “You are not going to see warfarin go away, because some physicians actually like it, and it is a lot less money. But you have to factor in the hassle factor and the drug interactions.”
Impact of Emerging Models of Care
In their discussion, the participants brought up the issue of incentives, and also emerging practice models such as Accountable Care Organizations (ACOs). The consensus among the participants was that increased incentives and the move away from fee-for-service toward population health management and value-based care should lead to improvements in overall care among patients with VTE and NVAF, including better management of patients who need anticoagulation therapy. This shift could include increasing the focus on improving TTRs for those on warfarin or considering the use of more expensive medications if their use reduces hospitalizations and overall cost. Dr Pezalla said, “I think the greatest opportunity lies in decreasing total cost of care, resulting in better outcomes.”
Many potential solutions are being considered that can improve outcomes, such as patient engagement, noted Dr Shaya. The concept is still relatively new, however. “There is a lot of talk about patient engagement now, and we do not know exactly what that translates into in terms of practice,” Dr Shaya said. Donald C. Balfour III, MD, FACP, commented that it is critical that patients be committed to improving their own health.
However, participants acknowledged that anticoagulation might not be a big readmission issue and that monitoring blood glucose levels, providing immunizations, and performing other services that are targets for compensation are of higher priority. It is important that there be incentives in place, noted several of the participants. ACOs are tasked with reducing the total cost of care, and thus may have the incentive to pay more attention to these populations. Currently, institutions are focusing their attention on areas where they may experience reimbursement penalties. “You have to align incentives,” Dr Balfour said. “It’s the only way.”
Conclusion
Anticoagulants are used to treat VTE, reduce the risk of recurrent VTE, and reduce the risk of stroke in NVAF. In VTE, the high recurrence rate in the first 3 weeks after the initiation of anticoagulant treatment emphasizes the need to quickly initiate and optimize anticoagulant therapy. To some providers and payers, the finding that the majority of VTE recurrences fall within the same critical period it takes INR to stabilize and reach therapeutic levels is an argument for the use of NOACs. The bridging requirements that are a part of warfarin therapy further complicate treatment, and also encourage the use of NOACs.
The need for monitoring INR and achieving INR control are additional complications of warfarin therapy in the VTE and NVAF populations. INR control is associated with reduced risk of major hemorrhage and thromboembolic events. However, good INR control is difficult to achieve, and well-coordinated systems tend to effect better INR control than isolated practices or less coordinated organizations.
INR control is more difficult in patients with a history of heart failure, diabetes, or previous stroke. In patients with multiple comorbidities, physicians tend to focus on the more clinically urgent problems, reserving anticoagulation initiation for a time when other priorities have been addressed. Physicians may also be reluctant to add to a patient’s pill and treatment burden.
Warfarin will likely remain a mainstay of anticoagulation. Despite the complexities of warfarin therapy, physicians are comfortable using warfarin. It is inexpensive, and some physicians like the fact that patients are coming in for INR monitoring, which allows for more frequent patient contact, and the ability to monitor compliance. While the availability of NOACs provides an opportunity for practitioners and payers to simplify treatment, warfarin therapy has its advantages as a standard of care.
Emerging practice models and the overall increasing emphasis on value-based care will likely play a role in anticoagulation therapy over the next several years. Efforts to reduce the total cost of care could lead health systems and payers to more closely examine standards of care issues in anticoagulation and the potential benefits of using NOACs if their use improves outcomes and is cost-effective.Author affiliations: Health Intelligence Partners, Chicago, IL (JB); Sharp Rees-Stealy Medical Group, San Diego, CA (DCB); Department of Pharmacotherapy, College of Pharmacy, University of Utah, Salt Lake City, UT (JEB); VRx Pharmacy Services, LLC, Salt Lake City, UT (JDD); EmblemHealth, New York, NY, and New York University, Stern School of Business, New York, NY (DBL); Jefferson Vascular Center, Thomas Jefferson University Hospital, Philadelphia, PA, and Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, PA (GJM); Pharmaceutical Policy and Strategy, Aetna, Hartford, CT (EJP); Center for Innovative Pharmacy Solutions, University of Maryland, School of Pharmacy, Baltimore, MD (FTS); Baptist Health Medical Group, Miami, FL (TV).
Funding source: This publication was developed by the staff of The American Journal of Managed Care, with editorial and financial support provided by Janssen Pharmaceuticals, Inc.
Author disclosure: Dr Dunn reports serving as a consultant/paid advisory board member for Daiichi Sankyo. Dr Merli reports receipt of grants from Portola Pharmaceuticals, Inc. Dr Villanueva reports employment with Baptist Health Medical Group and reports receipt of honoraria from American Regent, AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, GlaxoSmithKline, Janssen Pharmaceuticals, Inc., and Novo Nordisk. Drs Balfour, Berger, Biskupiak, Liotta, Pezalla, and Shaya have no relevant financial relationships with commercial interests to disclose.
Authorship information: Concept and design (DCB, JDD, GJM, EJP, FTS); acquisition of data (DCB); analysis and interpretation of data (DCB, GJM, JB, JEB, DBL, EJP, FTS); drafting of the manuscript (JEB, JDD, DBL, GJM, FTS, TV); critical revision of the manuscript for important intellectual content (JB, JEB, JDD, DBL, EJP, FTS); provision of study materials or patients (TV); administrative, technical, or logistic support (JB); and supervision (TV).
Address correspondence to: Jan Berger, MD, MJ. E-mail: berger.healthintell@ comcast.net.
- Kearon C, Akl EA, Comerota AJ, et al. Antithrombotic Therapy for VTE Disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2, suppl):e419S-e494S.
- January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;130(23):e199-e267.
- Coumadin® [package insert]. Princeton, NJ: Bristol-Myers Squibb Company; 2011.
- Douketis JD, Foster GA, Crowther MA, et al. Clinical risk factors and timing of recurrent venous thromboembolism during the initial 3 months of anticoagulant therapy. Arch Intern Med. 2000;160:3431-3436.
- The Columbus Investigators. Low-molecular-weight heparin in the treatment of patients with venous thromboembolism. N Engl J Med. 1997;337:657-662.
- Limone BL, Hernandez AV, Michalak D, Bookhart BK, Coleman CI. Timing of recurrent venous thromboembolism early after the index event: a meta-analysis of randomized controlled trials. Thromb Res. 2013;132:420-426.
- Wan Y, Heneghan C, Perera R, et al. Anticoagulation control and prediction of adverse events in patients with atrial fibrillation: a systemic review. Circ Cardiovasc Qual Outcomes. 2008;1:84-91.
- Nelson WW, Choi JC, Vanderpoel J, et al. Impact of co-morbidities and patient characteristics on international ratio control over time in patients with nonvalvular atrial fibrillation. Am J Cardiol. 2013;112:509-512.

