- Center on Health Equity & Access
- Clinical
- Health Care Cost
- Health Care Delivery
- Insurance
- Policy
- Technology
- Value-Based Care
A Review of the Current Management and Burden of Prurigo Nodularis in the United States
ABSTRACT
Prurigo nodularis (PN) is a chronic neural- and immune-mediated disease that is characterized by intense itch, history of skin scratching, and development of papulonodular lesions. These lesions can develop consequent to a cycle of itching and scratching associated with inflammation and changes in skin cells and nerve fibers (eg, pathogenic skin fibrosis, tissue remodeling, and chronic neuronal sensitization). Diagnosis of PN involves individual evaluation of clinical characteristics to identify disease and symptom severity. In the United States, adult patients with PN (estimated, < 90,000) are more likely to be older (age, 50-60 years); in addition, this disease is detected at higher rates in women and Black individuals relative to other demographic subgroups. Still, the small population of patients with PN exhibits considerably high use of health care resources and experiences considerable symptom burden and negatively impacted quality of life. Further, PN is associated with increased rates of a range of comorbid diseases compared with other inflammatory dermatoses (eg, atopic dermatitis, psoriasis). Adequate treatment must address both the neural and immunological component of the disease; there remains a great unmet need for safe and effective therapies that can reduce the burden of disease.
Am J Manag Care. 2023;29(suppl 5):S63-S72. https://doi.org/10.37765/ajmc.2023.89366
For author information and disclosures, see end of text.
Prurigo nodularis (PN) is a chronic neural- and immune-mediated disease that is associated with considerable disease burden.1-5 The disease is characterized by chronic pruritus, history of persistent skin scratching, and the appearance of papulonodular lesions on the skin.1 Compared with other chronically pruritic inflammatory dermatoses, PN is associated with more intense and frequent itching and greater impacts on quality of life (QOL).4 Although PN affects only a small population of patients, it is associated with high comorbidity burden and considerable health care costs and resource utilization.6-12 In the absence of formal guidelines for PN, many therapies are used off-label to reduce pruritus and heal lesions.1 There remains an unmet need for therapies that address the underlying drivers of PN. This review article aims to increase awareness and understanding of PN and define this unmet need.
Epidemiology
There are limited data on the epidemiology of PN.6 The International Classification of Diseases, 9th Revision (ICD-9) coding system, used in the United States before October 2015, did not provide a unique code for PN; therefore, identification of patients with PN for claims analysis at that time may have been less precise than it is now.6,13,14 Use of the more specific ICD-10-Clinical Modification (CM) coding system was mandated in the United States on October 1, 2015.14 The new ICD-10-CM code for PN has been validated, potentially allowing for more accurate identification of PN in epidemiologic analyses.6,15
One analysis using ICD-10-CM coding estimated the US prevalence of PN to be approximately 88,000 adults (72 / 100,000 adults) aged 18 to 64 years in 2016. Investigators analyzed administrative claims data from the IBM MarketScan Commercial Claims and Encounters Database (IBM Watson Health) to identify patients with PN, defined as those with at least 2 medical claims coded for PN from October 2015 through December 2016. Prevalence of PN was estimated using the 2016 US population as a reference. The true prevalence of PN and reduced generalizability of these results may have been underestimated because of a restriction of the study population (insured patients aged 18-64 years) and use of ICD-10-CM (PN-specific) coding that limited the study period and sample size.6
Certain populations are more likely to be affected by PN. Women appear to represent the majority of patients with PN (range, 51%-75%), according to several cohort and claims-based studies, although PN prevalence by gender may vary based on patient race.6-9,16 Older adults (mean age, 50-60 years) have shown to be more frequently affected. The results of a retrospective data analysis from the Symphony Health (2017) and LexisNexis PxDx (2017/2018) claims databases and Medicare (2017) found that the highest prevalence of PN was seen among the Medicare population (148.3 / 100,000 adults), which predominantly is comprised of older adults.13 The authors noted that data-entry errors may have led to misclassification in this type of analysis.
In addition, certain racial and ethnic populations may experience a higher prevalence of PN. The results of a retrospective analysis of data from 909 adult patients who received a diagnosis of PN at the Johns Hopkins Health System (JHHS) between 2012 and 2017 showed that Black patients were approximately 3 times more likely to receive a diagnosis of PN than were White patients (odds ratio [OR], 3.4; 95% CI, 2.9-3.9; P < .001). However, these results may not be generalizable to the general population or to those living in more remote areas, because this study focused on patients seen in 1 US hospital system.7
To identify any racial disparities in mortality risk among patients with PN, investigators analyzed data from 22,858 patients with at least 2 ICD-10 codes for PN in the health research network TriNetX between 1995 and 2020 (diagnoses prior to introduction of ICD-10 coding were mapped using Systematized Nomenclature of Medicine - Clinical Terms concepts).16 All patients with PN had an increased risk of mortality compared with controls, which the authors posited might have resulted from the higher comorbidity burden experienced by patients with PN. However, results also indicated that Black patients with PN had the highest risk of mortality (HR, 2.07; 95% CI, 1.64-2.61; P < .001) when compared with White, Hispanic, or Asian patients. The authors noted that more research is needed to identify why such disparities in mortality among patients with PN exist.16 Indeed, racial disparities in PN health outcomes may be associated not just with biologic factors, but also with social determinants of health, such as socioeconomic, environmental, societal, and health care access issues.17,18
Clinical Characteristics
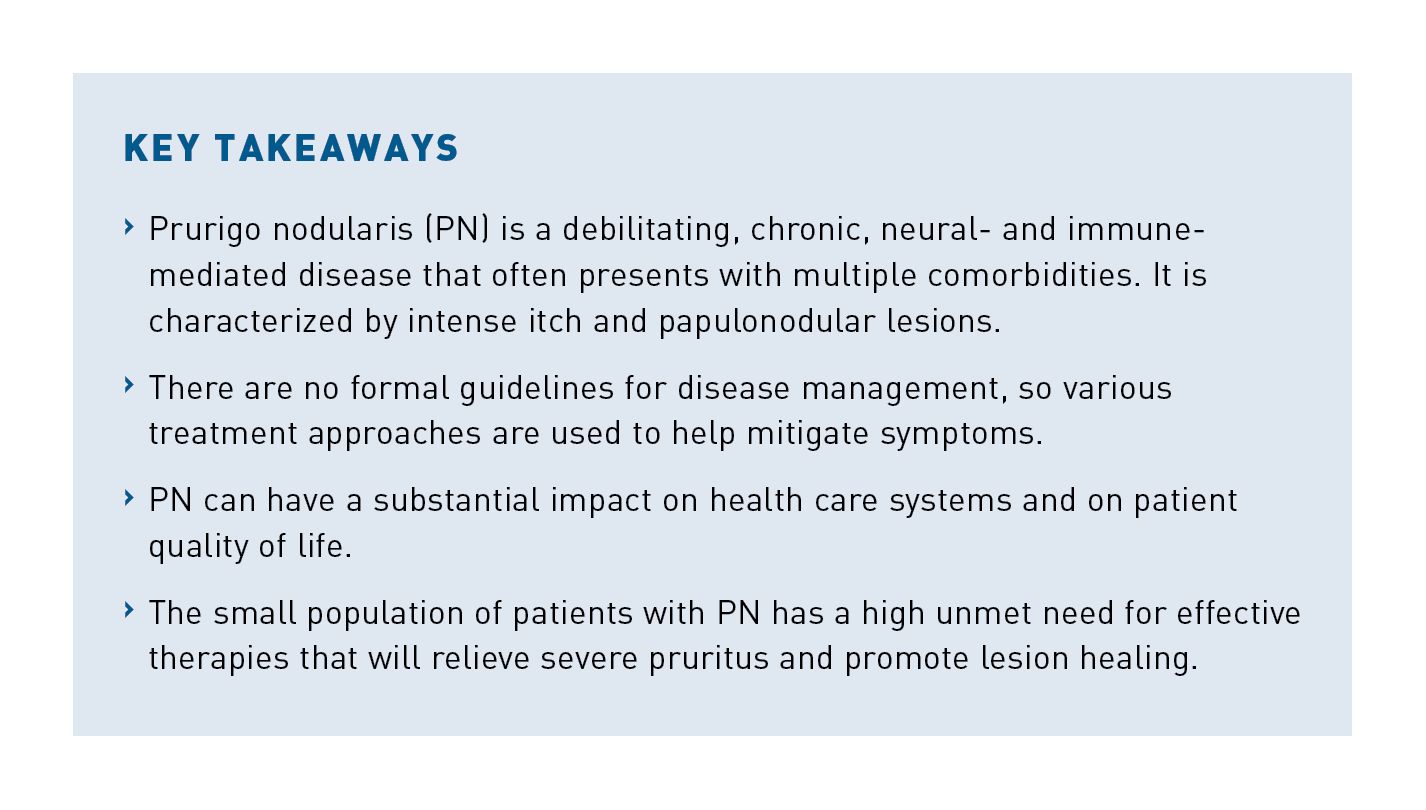
PN is a chronic inflammatory skin disease characterized by pruritus lasting longer than 6 weeks; a history or evidence of persistent skin scratching, picking, or rubbing; and the development of pruritic, hyperkeratotic papulonodular lesions (Table).1,2 These lesions can range from a few millimeters to 3 cm in size and often present with bilateral distribution on the torso and extremities, but they may be more localized in certain cases.1,19 Black patients with PN may experience larger, firmer, and more treatment-resistant lesions than do White patients.20 Patients present with very few to hundreds of lesions, which may be crusted or excoriated due to persistent scratching which induces development of additional lesions (Figure 121-23)in PN.1,2,19

Pruritus is a hallmark clinical manifestation of PN and occurs both in lesions and in areas of the skin between them; however, results from 2 separate patient-reported surveys showed that many patients with PN also experience sensations such as pain and burning.1,10,24 Up to 84.2% of patients with PN experienced additional sensations, with an average of 2.6 distinct sensations per patient.10,24 The approximate prevalence of additional sensations associated with PN included: prickling of the skin (62%), burning (53%-59%), pain (57%), stinging (47%-54%), tingling (35%), heat (21%), and cold (3%). The prevalence of sensations was not significantly related to the etiologic origin of PN or the type of sensation.24 Results may have been limited by retrospective study designs that excluded patients with PN who did not experience pruritus, by small study populations (N = 108 and N = 171), and by the subjectivity inherent in patient-reported data.10,24
Etiology and Pathogenesis
The underlying cause of PN is not known, but development of the disease may be driven by dysregulation of both neural and immune processes.1-3 Origination of PN may be associated with a heterogeneous set of etiologic factors, including dermatologic (eg, atopic dermatitis [AD]), systemic (eg, chronic renal failure, diabetes), and neuropsychiatric conditions.2,19,24 The results of a German retrospective analysis of 108 patients with PN showed that no underlying disease association could be found in 13% of cases; however, the majority of cases (59.3%) exhibited a combination of dermatologic, systemic, or neurologic origins.24 A lack of comprehensive clinical tests in all patients may have resulted in an inability to identify underlying disease. Independent of initial disease triggers or contributing etiologies, PN is self-perpetuating via a cycle of itching and scratching, once established.1,3,25
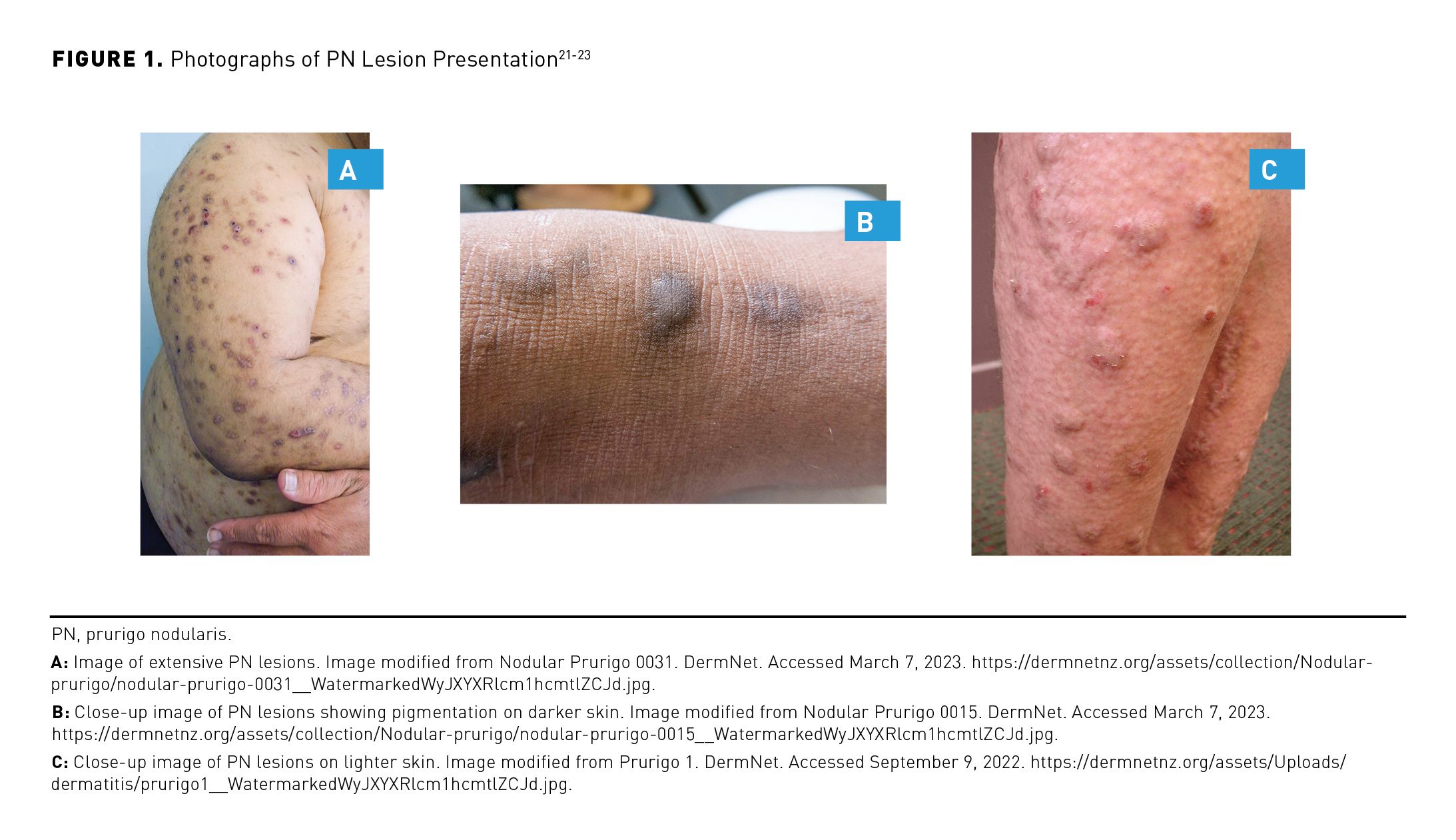
The pathogenesis of PN is not fully understood.2 However, histopathologic features of PN include both dermal and epidermal changes, such as papillary dermal fibrosis with vertically arranged collagen fibers and epidermal acanthosis with hypergranulosis.1 PN lesions show changes in a wide array of neural, immune, and skin resident cell types—including eosinophils, keratinocytes, and mast, endothelial, and dendritic cells—as well as a decreased density of intraepidermal nerve fibers and an increased density of dermal nerve fibers that may be associated with the chronic pruritus seen in PN.2,19,26,27 Results of a comparative transcriptomics study examining biopsies from patients with PN, AD, or psoriasis found that PN was associated with distinct dysregulation of gene signatures associated with fibroproliferative and neurovascular processes.28
In addition, type 2 inflammation may drive PN, resulting in a dysregulated relationship between neuronal, immune, and skin cells that promotes inflammation, pruritus, and tissue remodeling (Figure 2).3,27 Chronic scratching contributes to formation of characteristic PN lesions, wherein inflammation and skin remodeling may promote further release of pruritogenic factors and mediators of the type 2 immune response.3,19,29 Both adaptive and innate immune cells (eg, T helper type 2 (Th2) cells, mast cells, eosinophils, basophils, group 2 innate lymphoid [ILC2] cells, macrophages, and dendritic cells) can produce type 2 cytokines such as interleukin (IL)-4, IL-13, and IL-31.3,30 T cells release IL-31 in PN lesions; increased expression of this cytokine is highly correlated with itch in certain dermatologic diseases.27 In addition, IL-4 helps drive the differentiation of naïve T helper cells (Th0 cells) into Th2 cells.29,31 Through this mechanism, IL-4 also impacts IL-31 secretion, as Th2 cells are the major producers of IL-31.3,32,33
Chronic neuroinflammation and neuronal sensitization are key aspects of PN pathophysiology. The dermis of PN lesional skin shows evidence of increased calcitonin-gene related peptide and substance P (SP) expression which stimulate eosinophils to produce neuropeptides such as nerve growth factor that propagate neural hyperplasia and neuronal sensitization.27 IL-4, IL-13, and IL-31 are inflammatory mediators with direct actions on peripheral sensory neurons, where their signaling may contribute to chronic itch by modulating expression and/or sensitivity of itch receptors.3 Both IL-4 and IL-13 may sensitize sensory neurons to pruritogens such as IL-31. All 3 cytokines can enhance stimulation ofneurons identified in itch-scratch pathways and are key components of chronic itch.3,32
In addition to participating in itch signaling, IL-4, IL-13, and IL-31 can impact tissue remodeling and skin fibrosis in PN.3,26,30,33 IL-4 and IL-13 have been described to play a role in wound healing; however, persistent or excessive activity can contribute to profibrotic pathways that drive pathogenic fibrosis and collagen deposition.30 Furthermore, IL-31 may be a driver of skin cell proliferation and epidermal thickening.33 PN skin also shows increased activity of IL-22, a proinflammatory cytokine involved in skin inflammation and wound healing.3,34 Further, SP triggers mast cells to release VEGF, which promotes endothelial proliferation and vascularization that can contribute to PN nodule formation.27 Evidence suggests that other immune pathways, such as Th17 and Th22 axes, may also be dysregulated and contribute to PN pathophysiology.28 The therapeutic relevance of these pathways is still uncertain.
Comorbidities
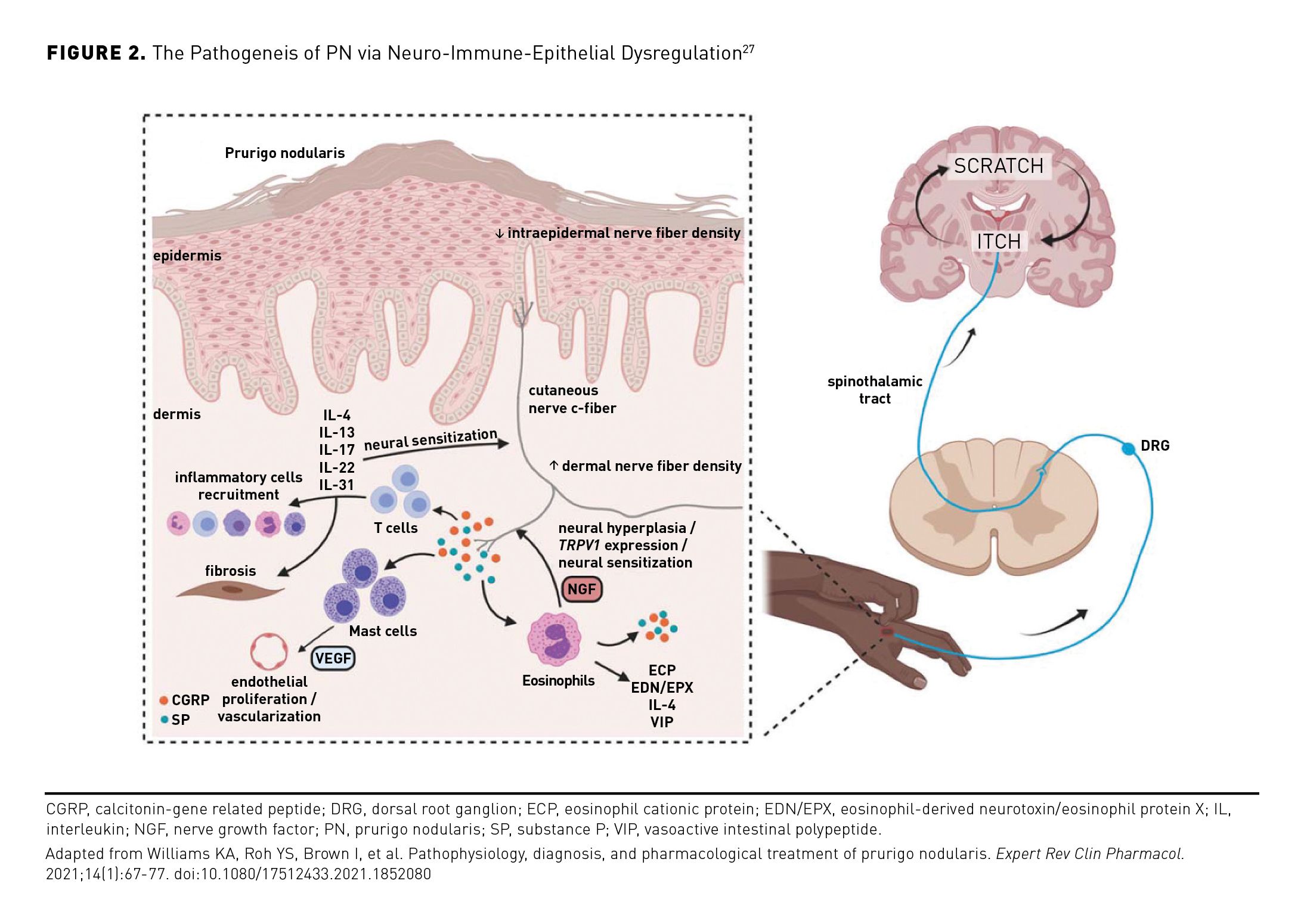
Patients with PN experience a higher comorbidity burden compared with those in the general population or with other inflammatory dermatoses, such as AD and psoriasis.6 In particular, PN is associated with several other type 2 inflammatory conditions, as well as a wide range of systemic and psychiatric conditions (eg, chronic kidney disease [CKD], cerebrovascular disease, depression, anxiety).6,7,29 There may be associations between certain comorbidities among patients with PN, indicating distinct comorbidity subgroups (eg, patients with a high prevalence of atopic conditions or chronic cardiopulmonary diseases).35
One study used nationally representative, private insurance claims data (2015-2019) of ICD-10-CM codes to identify patients with PN (defined as those with ≥ 2 medical claims for PN) and those with AD or psoriasis; subsequently, ICD-9-CM and ICD-10-CM codes were used to compare comorbidity burden among patients with PN, AD, or psoriasis and in matched controls. The results showed that in 2019, patients with PN had the highest comorbidity burden (as measured by the Charlson Comorbidity Index) as compared with matched controls or those with AD or psoriasis (mean [SD], 2.32 [2.84] vs 1.57 [2.42], 0.75 [1.52], and 1.71 [2.40], respectively). The retrospective design of this study may limit results, and further validation is required for use of ICD-10-CM codes to identify patients with PN.8
Comorbidities Associated With Type 2 Inflammation
Type 2 inflammation has been linked with many diseases and conditions, including AD, food allergies, asthma, and urticaria.3,29 Nearly one-fifth of patients with PN also experience a combination of eczema, asthma, and seasonal allergies referred to as “the atopic triad.”10
Studies routinely find associations between such comorbidities and PN; however, estimates of prevalence and risk have not been consistent across analyses. The results of the previously discussed study using IBM Watson Health data (2015-2016) found that compared with matched controls, patients with PN had nearly 9.5 times the risk of having AD, over 1.6 times the risk of having asthma, and over 2.5 times the risk of having urticaria.6 According to the previously discussed analysis of JHHS data (from 2012 to 2017), when compared with the general population, patients with PN had 72.2 times the risk of having AD and 10.3 times the risk of having asthma (both P < .001).7 The analysis did not support causality of these associations, which may have been a consequence of uncontrolled factors (eg, socioeconomic status).
Although both studies found that patients with PN have a substantially increased likelihood of these comorbidities, the magnitude of risk varied. Further, despite risk associations, comorbid prevalence of these diseases was low. Among patients with PN, the former study found the prevalence of AD to be 3.3%, of asthma to be 8.4%, and of urticaria to be 2.6%, whereas the latter study found the prevalence of AD to be 10.7% and of asthma to be 16.4%.6,7
Other Comorbidities
Patients with PN also are at an increased risk of comorbidities not associated with type 2 inflammation, such as psychiatric conditions and systemic diseases. For example, the results of a 2019 electronic survey in US adults with PN and associated pruritus lasting at least 6 weeks (N = 171) found that nearly half (45.6%) of participants had received a diagnosis of anxiety, and 16.4% had received a diagnosis of major depressive disorder.10 Indeed, the JHHS study results showed that patients with PN were over 16 times more likely than the general population to have depression and also were significantly more likely to have depression than were patients with AD or psoriasis (all comparisons P < .001).7 Note that this study did not consider dermatologic disease severity. Patients with PN also experience high rates of certain substance use disorders, which may be associated with self-medication for PN-related QOL disturbances (eg, chronic pruritus, depression, and pain).36
In addition, study results have shown that patients with PN have an increased likelihood of HIV infection, non-Hodgkin lymphoma, obesity, hypertension, type 2 diabetes, CKD, heart failure, cerebrovascular disease, coronary heart disease, and chronic obstructive pulmonary disease compared with matched controls or the general population.6,7 Higher rates of certain systemic diseases have been found in patients with PN versus those with AD or psoriasis (Figure 3),6 further highlighting the substantial comorbidity burden faced by these patients.
Certain racial disparities in comorbidity burden also have been noted among those with PN. Black patients with PN may have greater systemic inflammation than do White patients with PN, as reflected by higher erythrocyte sedimentation rate and C-reactive protein, ferritin, and blood eosinophil levels.20 One study observed faster progression of CKD among Black patients with PN than among White patients with PN.37 In addition, results from the JHHS study showed a statistically significant association between PN and the following conditions among Black patients (n = 449): HIV infection (n = 122), ischemic heart disease (n = 87), and hypertension (n = 248) (all P < .001).7 These associations were not present among White patients with PN in the study. As previously noted, this study focused on patients seen in 1 US hospital; furthermore this study did not control for social determinants of health, which may confound results. Therefore, results may not be generalizable.7
Diagnosis of PN
Identification of PN and of disease severity is contingent upon individual patient assessment of symptoms, disease burden, and physical examination. Several diseases may present similarly to PN. A skin biopsy may be performed to rule out other dermatologic diagnoses. Skin scrapings may be examined to rule out scabies or underlying fungal infections, and direct immunofluorescence may help to exclude cutaneous autoimmune disorders. As with other chronic itch presentations, clinicians may screen for evidence of organ dysfunction and systemic disorders and consider laboratory testing to rule out the presence of underlying infectious (eg, HIV, hepatitis B or C) or systemic (eg, diabetes) etiologies. It should be noted that PN is primarily a clinical diagnosis. Disease severity should be assessed by investigating intensity of pruritus and by identifying the number and firmness of lesions in each patient. Disease burden—including patient QOL, sleep disturbances, depression/anxiety, and associated comorbidities (Table)—also should be assessed in each patient.1
Current Treatments
There are no formal US guidelines for management of PN; however, consensus treatment recommendations are available from a 2019 US expert panel.1 Treatment for PN largely focuses on decreasing pruritus to heal lesions.1,2 There is variability in selection and dosing regimens for therapeutic agents, and many therapies are used off-label.1
According to the expert panel consensus recommendations, the treatment approach for PN should optimally be multimodal and involve individualized plans that consider patient characteristics (eg, age, comorbidities, and PN severity and manifestations), and impact on patient QOL and adverse events (AEs), rather than those that rely on a stepwise approach.1,19 Treatment also should simultaneously address any contributors to disease, if known.19 As such, both neural and immunologic therapies often are used.1 Current treatments may be associated with AEs of varying severity.1,19 In most cases, long-term treatment is required; however, authors of the US consensus statement on PN shared that according to clinical evidence and their experience, some treatments are associated only with short-term efficacy.1,19
The US expert panel provided a recommended treatment ladder that comprises 4 tiers.1 Depending on clinical presentation and disease severity, patients with PN may begin treatment in any tier and move up or down the ladder based on treatment response (Figure 4).1 As with many inflammatory skin conditions, the foundation of treatment for PN involves gentle skin care and use of topical emollients.1,19 However, controlling PN symptoms may require the use of additional treatments as described in the tiered treatment ladder.
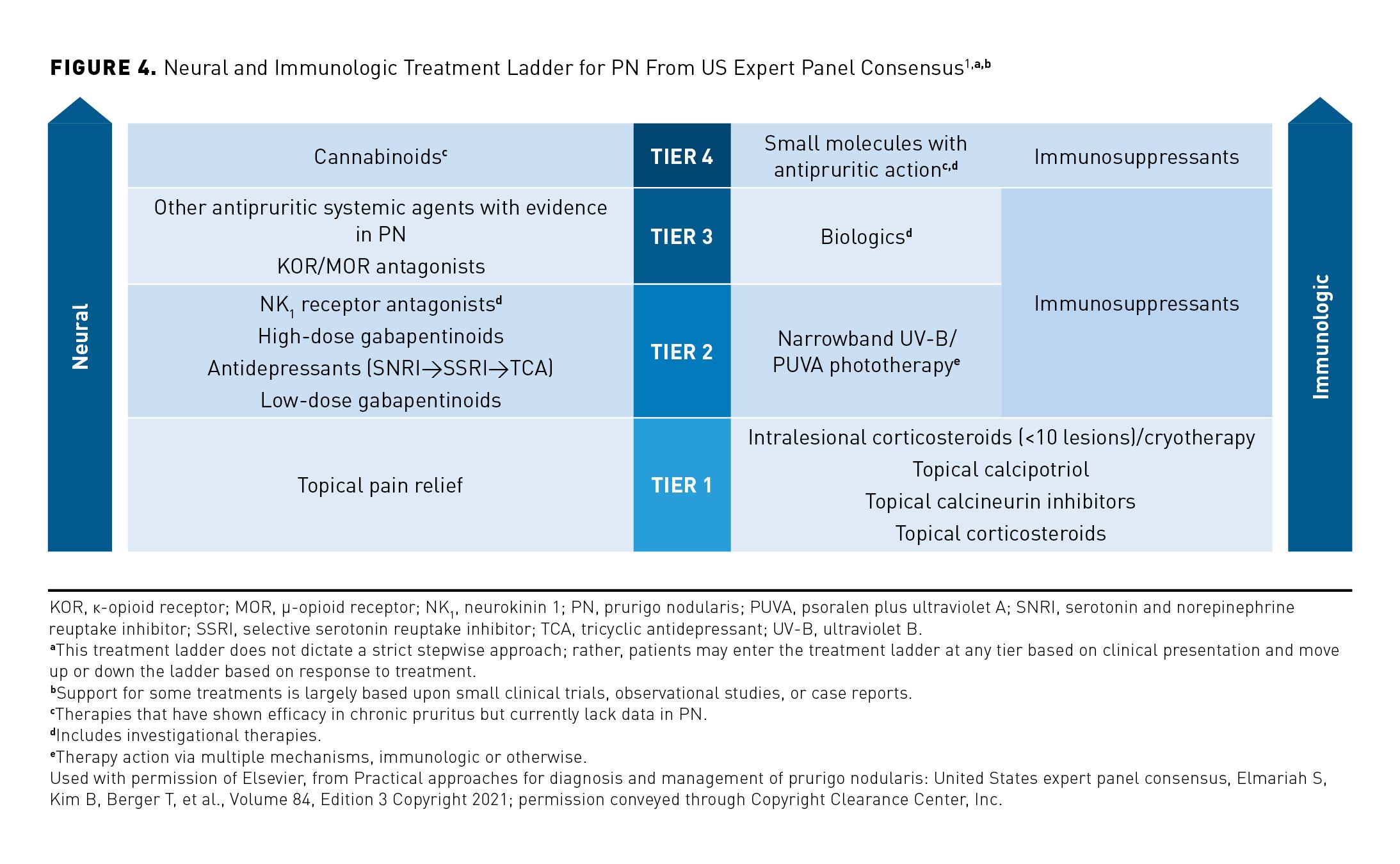
Tier 1 treatments include topical therapies with various mechanisms of action.1 These treatments may lack evidence for long-term use in PN. Tier 2 treatments include widespread skin-directed or systemic therapies; these include phototherapy, antidepressants, gabapentinoids, NK1 receptor antagonists, and steroid-sparing immunosuppressants.1 Access to phototherapy may be a challenge for some patients; this treatment may be required multiple times per week for months or years, and relapse after treatment also is possible.38 Tier 3 therapies include biologics or other systemic agents with antipruritic action, drugs that activate or block certain opioid receptors, and steroidal or steroid-sparing immunosuppressants.1 Systemic corticosteroid treatment has limited utility in PN due to the potentially serious AEs associated with high-dose or long-term treatment.1,39 Tier 4 therapies have known antipruritic effects; however, at the time of the consensus statement’s publication (2021), data on the use of such agents (eg, systemic or topical cannabinoids, small molecule therapies) in treating PN were lacking.1
Economic, Symptomatic, and Humanistic Burden of PN
High health care costs and resource utilization, extremely intense and frequent pruritus, and diminished QOL are substantial burdens experienced by patients with PN.
Economic Burden
PN is associated with a considerable economic burden, including high outpatient care rates and increased risk of emergency department (ED) admissions, as well as costs and length of stay for inpatient visits. The societal lifetime burden of PN on the US health care system was estimated to be $38.8 billion in 1 study; this approximation was based on prevalence estimates from the literature and an individual lifetime burden of $323,292 (from an average 6.5 quality-adjusted life-years lost and a willingness-to-pay threshold of $50,000).9
Analysis of results from the 2019 electronic survey in patients with PN (mean age [SD], 52.3 [13.2] years) found that on average, respondents visited their physician 6.3 (SD, 3.3) times over the previous year.10 According to a data brief from the US Centers for Disease Control and Prevention that analyzed data from the National Ambulatory Medical Care Survey, there were 267 (SD, 12) office-based physician visits per 100 persons of all ages in the United States (or approximately 2.7 outpatient visits / person) in 2018.40 Among individuals between the ages of 45 and 64 years, there were 302 (SD, 18) outpatient visits per 100 persons (or approximately 3 outpatient visits / person) that year.40 Overall in 2018, the average person in the general population made less than half of the visits reported by patients with PN in the 2019 survey, highlighting the high outpatient resource use associated with PN.
The survey of patients with PN also found that 88.3% of patients visited a dermatologist over the previous year.10 Indeed, the previously described analysis of retrospective private insurance claims data (2015-2019) that investigated comorbidity burden in terms of health care resource utilization found that patients with PN had more claims for dermatology visits than did controls or those with AD or psoriasis (visits / year, 1.87 vs 0.31, 0.75, and 1.38, respectively).8
PN also is associated with an increased incidence of hospital admission. Investigators estimated the number of ED visits made by patients with PN (identified via ICD-10-CM coding) using the cross-sectional 2016 National Emergency Department Sample from the Healthcare Cost and Utilization Project, which captured more than 32 million visits in the United States. Patients with PN were significantly more likely to be admitted as inpatients to the hospital than were those in the general patient population (67% vs 13%, respectively) (OR, 67.4; 95% CI, 61.5-72.7; P < .001). In 2016, among patients with PN, the total cost of ED services nationally was $4,377,553 (SD, $740,743), and the average cost for ED services was $3206 (SD, $397). The authors drew a comparison between their results and ED service costs for patients with AD—the average ED service costs for patients with PN were substantially higher than those reported in the literature for patients with AD, and that difference may be due to the high rates of serious systemic illness and hospital admission in patients with PN. Furthermore, in patients with a secondary diagnosis of PN, the 2 most common primary diagnoses were sepsis and cellulitis.11
Compared with inpatients without PN, those with PN experienced increased cost of care and length of hospitalization. Investigators on a separate study analyzed the inpatient burden of PN in the United States using 2016 data from the National Inpatient Sample, which provides a stratified sample of 20% of all US inpatient hospitalizations. Patients with PN were identified using ICD-10-CM coding. Length of stay and cost of care data for these patients were compared with data from patients with no diagnosis of PN (ie, control group). For patients with PN, there were approximately 3.7 inpatient visits per 100,000 total discharges in 2016. Compared with the general inpatient population, those with PN were more likely to be of Black (P < .001), Hispanic (P = .02), or Asian (P = .003) heritage (reference White heritage). Length of hospital stay was significantly longer for patients with PN vs those without the disease (mean [SD], 6.51 [0.37] days vs 4.62 [0.02] days; P < .001). In addition, the average inpatient cost of care in 2016 also was higher for patients with PN vs those without PN ($14,772 [$964] vs $11,728 [$106]; P < .001). As with the previous analysis, data from this study showed that the 2 most common primary reasons for admission among patients with PN were sepsis and cellulitis.12
The results from these health care cost and resource use studies may be limited due to study designs, small sample sizes, low recognition of PN by nondermatologic specialties, and the inability to determine the economic effects of disease severity or treatment.8-12
Symptom Burden
Patients with PN experience considerable symptom burden that can negatively impact QOL. Results of the previously described 2019 electronic survey of 171 patients with PN showed that 35.7% of respondents experienced pruritus for 1 to 5 years, and 32.2% experienced pruritus for longer than 10 years. More than 90% of patients reported having at least 10 pruritic nodules, and of patients in whom itch location was assessed (n = 88), 67% reported itch being localized both to lesions and to intervening skin.10
Patients with certain inflammatory dermatoses experience moderate to severe intensity of pruritus; however, study results indicate that pruritus experienced by patients with PN is significantly worse than in patients with other pruritic conditions.4 Results from a multicenter European cross-sectional study of 552 adult patients with chronic pruritus and inflammatory dermatoses (eg, PN, AD, contact dermatitis, psoriasis vulgaris, lichen planus, or mycosis fungoides / Sézary syndrome) who were enrolled from 2015 to 2016 found that patients with PN reported a significantly greater intensity (P < .01) and frequency (P < .05) of pruritus than did those patients with other pruritic conditions. Among patients with PN, more than half (56.5%) reported an increase in pruritus after scratching, and 77.1% reported experiencing pruritus often or always in the evening. The authors pointed to these examples to explain the higher QOL burden experienced by affected patients. Indeed, 60.1% of patients with PN reported that they were often or always impaired in their everyday life activities (P < .01). Patients with noninflammatory pruritus were not included, and data were gathered from 9 mostly urban single centers in 9 European countries; thus, results may not be representative.4
Impact on Quality of Life
PN is associated with a substantial negative impact on patient QOL, according to the results of a systematic review and meta-analysis of 12 publications from Europe and Asia that were pulled from OVID MEDLINE, EMBASE, SCOPUS, and Web of Science; these publications were available from database inception through April 23, 2020. The most common QOL instrument used was the Dermatology Life Quality Index (DLQI), which includes 10 questions scored on a scale of 0 to 30 (patient QOL, from no effect [0-1] to extremely large effect [21-30]). From the 9 studies assessing DLQI, the random-effects mean score was 13.8 (95% CI, 10.6-16.9), denoting the very large effect of PN on patient QOL. Limitations of this analysis included a lack of consistent disease definition among studies analyzed, of individual patient data for meta-analysis, and of validated tools for measuring QOL in patients with PN.5
Patients with PN experience significantly worse QOL compared with the general population (P < .001). Investigators used the generic Ontario Health Utilities Index Mark 3 (HUI3) health utility instrument—where a score of 0.00 is death and of 1.00 is perfect health—to compare the QOL burden experienced by adults in the general population to that experienced by 36 adult patients who presented with a confirmed PN diagnosis at the Johns Hopkins Itch Clinic. The data on those in the general US population (n = 4187) were gathered from the cross-sectional 2002-2003 joint Canada/United States Survey of Health. The results indicated that patients with PN had significantly worse average (mean [SD]) HUI3 scores than did those in the general population (0.52 [0.06] vs 0.86 [0.003], respectively; P < .001). Furthermore, after adjustment for age, race, and history of multiple diseases, PN was still associated with significantly worse scores in dexterity (P = .003), cognition (P = .001), and ambulation, emotion, and pain (all P < .001). Notably, PN was associated with worse QOL than were asthma, diabetes, and stroke. Generalizability of results in this study is limited due to the small sample size in this study (common in PN studies due to rarity of PN) and the design of the study, which gathered data from a single tertiary-care center and lacked the ability to measure QOL over time following PN treatment.9
Finally, the substantial QOL burden experienced by patients with PN was further highlighted in the previously discussed multicenter European cross-sectional study of patients with chronic pruritus and various inflammatory dermatoses.4 Not only did patients with PN report significantly greater frequency (P < .05) and intensity (P < .01) of itch than did the patients with other inflammatory dermatoses, but they also indicated a significantly greater impairment in QOL due to itch, as measured by the pruritus-specific ItchyQOL instrument.4 The ItchyQOL consists of 22 items focused on pruritus-specific symptoms, functional limitations, and emotions experienced over the previous 7 days to provide a total score ranging from 22 to 110.4,41 Among all patients, including those with PN, the mean (SD) ItchyQOL score was 65.3 (19.1).4 The mean score reported by patients with PN was 74.1 (15.4), indicating a significantly greater effect on QOL than that experienced by the patients with other inflammatory dermatoses (P < .001).
Conclusions
The pathophysiology of PN has not been fully elucidated. It is driven, in part, by type 2 inflammation that results in a dysregulated relationship between neuronal, immune, and skin cells via downstream effects of IL-4, IL-13, and IL-31, among other signaling molecules. Patients with PN experience an intense cycle of itching and scratching that leads to the development of pruritic, fibrotic and hyperkeratotic lesions. There are no formal guidelines to manage PN, but various treatment approaches are used to mitigate its debilitating symptoms, which can have a substantial impact on patient QOL and contribute to substantially increased health care resource utilization. There is an unmet need for approved treatments that can be used in the long term to relieve severe pruritus and encourage the healing of lesions.
Authorship affiliation: Emory University (SSC), Atlanta, GA; Department of Veterans Affairs Medical Center (SSC), Decatur, GA.
Funding source: This supplement was sponsored by Sanofi and Regeneron Pharmaceuticals, Inc.
Author disclosure: Dr Chisolm reports serving as a paid advisory board member for Sanofi, Regeneron Pharmaceuticals, Inc., and Galderma.
Authorship information: Concept and design (SSC); drafting of the manuscript (SSC), critical revision of the manuscript for important intellectual content (SSC).
Address correspondence to: Sarah S. Chisolm, MD. Emory University, 1525 Clifton Rd. NE, 1st floor, Atlanta, GA 30322. Email: Sarah.chisolm@emory.edu
References
- Elmariah S, Kim B, Berger T, et al. Practical approaches for diagnosis and management of prurigo nodularis: United States expert panel consensus. J Am Acad Dermatol. 2021;84(3):747-760. doi:10.1016/j.jaad.2020.07.025
- Zeidler C, Ständer S. The pathogenesis of prurigo nodularis—‘super-itch’ in exploration. Eur J Pain. 2016;20(1):37-40. doi:10.1002/ejp.767
- Garcovich S, Maurelli M, Gisondi P, Peris K, Yosipovitch G, Girolomoni G. Pruritus as a distinctive feature of type 2 inflammation. Vaccines (Basel). 2021;9(3):303. doi:10.3390/vaccines9030303
- Steinke S, Zeidler C, Riepe C, et al. Humanistic burden of chronic pruritus in patients with inflammatory dermatoses: results of the European Academy of Dermatology and Venereology Network on Assessment of Severity and Burden of Pruritus (PruNet) cross-sectional trial. J Am Acad Dermatol. 2018;79(3):457-463.e5. doi:10.1016/j.jaad.2018.04.044
- Janmohamed SR, Gwillim EC, Yousaf M, Patel KR, Silverberg JI. The impact of prurigo nodularis on quality of life: a systematic review and meta-analysis. Arch Dermatol Res. 2021;313(8):669-677. doi:10.1007/s00403-020-02148-0
- Huang AH, Canner JK, Khanna R, Kang S, Kwatra SG. Real-world prevalence of prurigo nodularis and burden of associated diseases. J Invest Dermatol. 2020;140(2):480-483.e4. doi:10.1016/j.jid.2019.07.697
- Boozalis E, Tang O, Patel S, et al. Ethnic differences and comorbidities of 909 prurigo nodularis patients. J Am Acad Dermatol. 2018;79(4):714-719.e3. doi:10.1016/j.jaad.2018.04.047
- Wongvibulsin S, Sutaria N, Williams KA, et al. A nationwide study of prurigo nodularis: disease burden and healthcare utilization in the United States. J Invest Dermatol. 2021;141(10):2530-2533.e1. doi:10.1016/j.jid.2021.02.756
- Whang KA, Le TK, Khanna R, et al. Health-related quality of life and economic burden of prurigo nodularis. J Am Acad Dermatol. 2022;86(3):573-580. doi:10.1016/j.jaad.2021.05.036
- Aggarwal P, Choi J, Sutaria N, et al. Clinical characteristics and disease burden in prurigo nodularis. Clin Exp Dermatol. 2021;46(7):1277-1284. doi:10.1111/ced.14722
- Whang KA, Gabriel S, Chavda R, Kwatra SG. Emergency department use by patients with prurigo nodularis in the United States. J Am Acad Dermatol. 2021;84(4):1138-1140. doi:10.1016/j.jaad.2020.06.1002
- Whang KA, Kang S, Kwatra SG. Inpatient burden of prurigo nodularis in the United States. Medicines (Basel). 2019;6(3):88. doi:10.3390/medicines6030088
- Ständer S, Augustin M, Berger T, et al. Prevalence of prurigo nodularis in the United States of America: a retrospective database analysis. JAAD Int. 2020;2:28-30. doi:10.1016/j.jdin.2020.10.009
- International Classification of Diseases, (ICD-10-CM/PCS) Transition – Background. Centers for Disease Control and Prevention. Reviewed November 6, 2015. Accessed October 10, 2022. https://www.cdc.gov/nchs/icd/icd10cm_pcs_background.htm
- Roh YS, Marani M, Choi U, et al. Validation of International Classification of Diseases Tenth Revision code for prurigo nodularis. J Am Acad Dermatol. 2022;87(2):482-484. doi:10.1016/j.jaad.2021.10.026
- Sutaria N, Adawi W, Brown I, et al. Racial disparities in mortality among patients with prurigo nodularis: a multi-center cohort study. J Am Acad Dermatol. 2022;86(2):487-490. doi:10.1016/j.jaad.2021.09.028
- Sutaria N, Semenov YR, Kwatra SG. Understanding racial disparities in prurigo nodularis. J Am Acad Dermatol. 2022;87(3):e111-e112. doi:10.1016/j.jaad.2022.05.014
- About social determinants of health (SDOH). Centers for Disease Control and Prevention. March 10, 2021. Accessed October 10, 2022. https://www.cdc.gov/socialdeterminants/about.html
- Zeidler C, Yosipovitch G, Ständer S. Prurigo nodularis and its management. Dermatol Clin. 2018;36(3):189-197. doi:10.1016/j.det.2018.02.003
- Sutaria N, Alphonse MP, Marani M, et al. Cluster analysis of circulating plasma biomarkers in prurigo nodularis reveals a distinct systemic inflammatory signature in African Americans. J Invest Dermatol. 2022;142(5):1300-1308.e3. doi:10.1016/j.jid.2021.10.011
- Nodular Prurigo 0031. DermNet. Accessed March 7, 2023. https://dermnetnz.org/assets/collection/Nodular-prurigo/nodular-prurigo-0031__WatermarkedWyJXYXRlcm1hcmtlZCJd.jpg
- Nodular Prurigo 0015. DermNet. Accessed March 7, 2023. https://dermnetnz.org/assets/collection/Nodular-prurigo/nodular-prurigo-0015__WatermarkedWyJXYXRlcm1hcmtlZCJd.jpg
- Prurigo 1. DermNet. Accessed October 10, 2022. https://dermnetnz.org/assets/Uploads/dermatitis/prurigo1__WatermarkedWyJXYXRlcm1hcmtlZCJd.jpg
- Iking A, Grundmann S, Chatzigeorgakidis E, Phan NQ, Klein D, Ständer S. Prurigo as a symptom of atopic and non-atopic diseases: aetiological survey in a consecutive cohort of 108 patients. J Eur Acad Dermatol Venereol. 2013;27(5):550-557. doi:10.1111/j.1468-3083.2012.04481.x
- Kwatra SG. Breaking the itch-scratch cycle in prurigo nodularis. N Engl J Med. 2020;382(8):757-758. doi:10.1056/NEJMe1916733
- Weigelt N, Metze D, Ständer S. Prurigo nodularis: systematic analysis of 58 histological criteria in 136 patients. J Cutan Pathol. 2010;37(5):578-586. doi:10.1111/j.1600-0560.2009.01484.x
- Williams KA, Roh YS, Brown I, et al. Pathophysiology, diagnosis, and pharmacological treatment of prurigo nodularis. Expert Rev Clin Pharmacol. 2021;14(1):67-77. doi:10.1080/17512433.2021.1852080
- Sutaria N, Alphonse MP, Roh YS, et al. Cutaneous transcriptomics identifies fibroproliferative and neurovascular gene dysregulation in prurigo nodularis compared with psoriasis and atopic dermatitis. J Invest Dermatol. 2022;142(9):2537-2540. doi:10.1016/j.jid.2022.02.010
- Gandhi NA, Bennett BL, Graham NMH, Pirozzi G, Stahl N, Yancopoulos GD. Targeting key proximal drivers of type 2 inflammation in disease. Nat Rev Drug Discov. 2016;15(1):35-50. doi:10.1038/nrd4624
- Nguyen JK, Austin E, Huang A, Mamalis A, Jagdeo J. The IL-4/IL-13 axis in skin fibrosis and scarring: mechanistic concepts and therapeutic targets. Arch Dermatol Res. 2020;312(2):81-92. doi:10.1007/s00403-019-01972-3
- Agnello D, Lankford CS, Bream J, et al. Cytokines and transcription factors that regulate T helper cell differentiation: new players and new insights. J Clin Immunol. 2003;23(3):147-161. doi:10.1023/a:1023381027062
- Oetjen LK, Mack MR, Feng J, et al. Sensory neurons co-opt classical immune signaling pathways to mediate chronic itch. Cell. 2017;171(1):217-228.e13. doi:10.1016/j.cell.2017.08.006
- Singh B, Jegga AG, Shanmukhappa KS, et al. IL-31-driven skin remodeling involves epidermal cell proliferation and thickening that lead to impaired skin-barrier function. PLoS One. 2016;11(8):e0161877. doi:10.1371/journal.pone.0161877
- Belzberg M, Alphonse MP, Brown I, et al. Prurigo nodularis is characterized by systemic and cutaneous T helper 22 immune polarization. J Invest Dermatol. 2021;141(9):2208-2218.e14. doi:10.1016/j.jid.2021.02.749
- Wongvibulsin S, Parthasarathy V, Pahalyants V, et al. Latent class analysis identification of prurigo nodularis comorbidity phenotypes. Br J Dermatol. 2022;186(5):903-905. doi:10.1111/bjd.20957
- Taylor MT, Bordeaux ZA, Deng J, et al. Association between prurigo nodularis and substance use disorders. Br J Dermatol. 2022;10.1111/bjd.21676. doi:10.1111/bjd.21676
- Sutaria N, Marani M, Choi J, et al. Racial differences in dysregulation of the renin-angiotensin-aldosterone system in patients with prurigo nodularis. J Dermatol Sci. 2022;105(2):130-136. doi:10.1016/j.jdermsci.2022.02.004
- Zhong CS, Elmariah SB. Phototherapy for itch. Dermatol Clin. 2020;38(1):145-155. doi:10.1016/j.det.2019.08.008
- Rice JB, White AG, Scarpati LM, Wan G, Nelson WW. Long-term systemic corticosteroid exposure: a systematic literature review. Clin Ther. 2017;39(11):2216-2229. doi:10.1016/j.clinthera.2017.09.011
- Ashman J, Santo L, Okeyode T. Characteristics of office-based physician visits, 2018. Centers for Disease Control and Prevention. May 2021. Accessed August 9, 2022. https://www.cdc.gov/nchs/products/databriefs/db408.htm
- Desai NS, Poindexter GB, Monthrope YM, Bendeck SE, Swerlick RA, Chen SC. A pilot quality-of-life instrument for pruritus. J Am Acad Dermatol. 2008;59(2):234-244. doi:10.1016/j.jaad.2008.04.006
